Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Clin Assoc Prof Amanda Oakley, Hamilton, New Zealand, 2008.
Introduction
Ingredients
Hydroquinone
Topical retinoids
Cysteamine cream
Botanicals
Other agents
Topical corticosteroids
Mercury
Bleaching or skin lightening creams or ointments are widely used worldwide either to attempt to remove localised dark patches (eg, melasma or postinflammatory hyperpigmentation) or as a fashion trend aiming to reduce normal melanin in the skin.
A bleaching cream may contain a variety of ingredients. Some of these are more effective than others. In many areas, unregulated products are sold, often without listing their contents or they are labelled incorrectly. They may be safe but completely ineffective, or the chemicals may result in side effects and toxicity. The risks depend on which ingredient is being applied to the skin, in what concentration, over what area, and for how long it is used.
Skin lightening agents may include:
Hydroquinone is an effective skin lightening agent. The recommended concentration over the counter is 2%, but up to 4% is available from a dermatologist in some countries. It should be used daily for no more than 6 months.
Exogenous ochronosis is the main risk of excessive use of hydroquinone. This results in an irregular blue-black staining affecting sun-exposed skin and nails.
In some subjects, excessive use of hydroquinone in combination with certain foods in the diet (fish, eggs, offal, beans) can result in an unpleasant fish odour in the body secretions such as sweat and urine (trimethylaminuria).
Hydroquinone is sometimes given another name, such as:
Monobenzyl ether of hydroquinone is a strong derivative of hydroquinone that can cause irreversible complete depigmentation of the skin (white patches).
Tretinoin is the main topical retinoid that has been used in skin lightening products. It thins the skin, increasing the penetration of other agents. as well as having a direct effect in reducing melanisation. It is a prescription medication because of potential risk in pregnancy. It can be quite irritating and may cause contact irritant dermatitis.
Cysteamine cream is applied for 15 minutes each day for up to 12 weeks, then twice weekly for maintenance. It can cause temporary burning and redness, and may also cause dryness and irritation, relieved by applying an emollient.
New active skin lightening compounds isolated from plants are being added to modern cosmetics. They appear to inhibit the production of melanin without being toxic to the melanocyte (tyrosinase inhibitors). It is not yet known which preparations are the most effective. Active ingredients include:
Other agents in use for their skin lightening effect include:
Unregulated skin lightening creams may include many other ingredients. These may be relatively safe (for example, lemon juice), toxic (camphor), irritating (detergents) or likely to provoke allergy (hair dye). Complications may include:
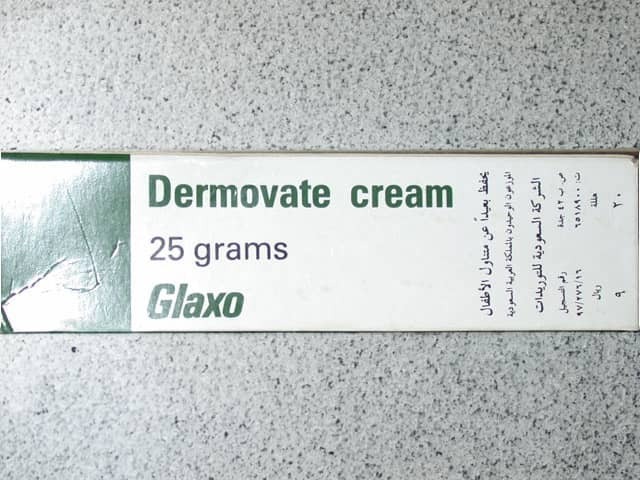
Dermovate cream
Dermovate cream
Topical corticosteroids lighten the skin by the following mechanisms.
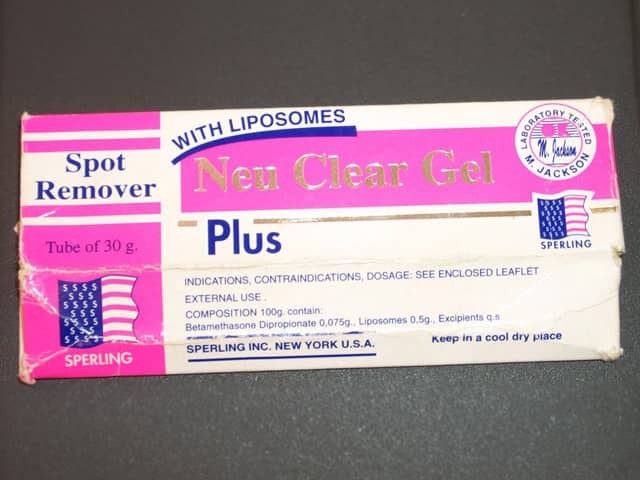
In New Zealand and many other countries, stronger topical corticosteroids are regulated and can only be obtained with a doctor's prescription. Products containing betamethasone valerate, fluocinonide and clobetasol propionate can be purchased over the counter from a pharmacy or from drug vendors in a marketplace in other countries.
Potent topical steroids have a wide range of local side effects including skin thinning and atypical fungal infections (tinea incognito). When used over large areas for prolonged periods, they may risk serious internal disease from hypopituitarism. Steroid addiction syndrome results in folliculitis and steroid rosacea.

Stretch marks

Folliculitis
Mercury was used as mercurous chloride, oxide and ammoniated mercury in many cosmetics and toiletries in the early part of the 20th century before it was realised it caused toxicity. It is still found in some skin lightening creams because mercury inactivates the enzyme that leads to the production of melanin. These products should not be used and are illegal in many countries including the USA and New Zealand.
Longterm application of mercurial products to the skin makes the skin and nails darker because the mercury is deposited in the epidermis, hair follicles and dermis.
Mercury poisoning results in acute and chronic toxicity including acrodynia, as well as neurological and kidney damage.