Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2007.
Ultraviolet-B (UVB) is the name given to the waveband of electromagnetic radiation ranging from 290 to 320 nm. Solar UVB is responsible for the majority of sunburn and is the main cause of sun damage and skin cancer. It is greatest at solar noon (1.30 pm in summer in New Zealand), at shorter latitudes, higher altitude and on clear days. It is blocked by window glass.
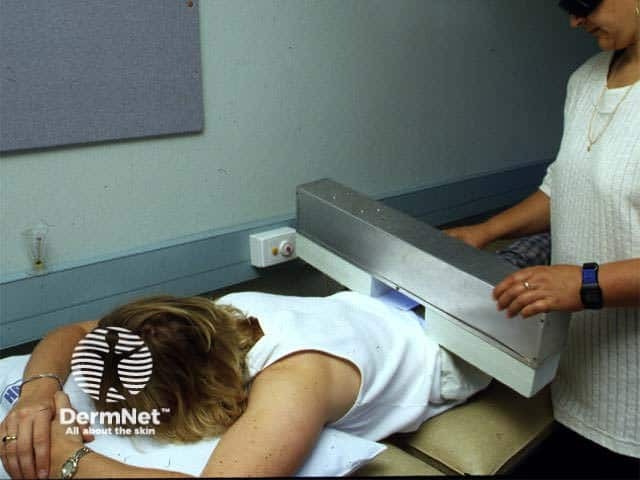
UVB phototherapy is effective in clearing or controlling a variety of skin diseases. It is available at the larger public hospitals and some private dermatologists' offices in New Zealand. Phototherapists are most often registered nurses but may also be physiotherapists or unqualified staff under the supervision of a dermatologist.
Phototherapy units in New Zealand are full-body cabinets containing 6-foot long, 100W fluorescent low-pressure mercury bulbs. Broadband UVB lamps have red identification markings (eg, FS72T12UVBHO) and narrowband lamps have brown markings. Older units supply broadband UVB (BB-UVB) with TL100/12 lamps, but increasingly these are being converted to or replaced by narrowband sources (NB-UVB) with TL100/01 lamps, often with 48 or 56 bulbs in the cabinet. Original 4-bulb Theraktin units are being phased out but may still be in use.
Modern units have integrated dosimetry and the time to deliver the correct dose is automatically calculated. For older units, irradiance is checked manually prior to treatment using a specific UVB dosimeter and the treatment time for a specific dose determined according to a spreadsheet.
Bulb markings Photherapy 



Psoriasis is the most common skin disease treated with UVB. NB-UVB phototherapy clears about 75% of patients, where clearance is defined as 90% or greater reduction in the extent of psoriasis compared to baseline. The number of treatments required ranges from 10 to 40, delivered two to five times weekly. BB-UVB clears a smaller proportion and a greater number of treatments may be required.
UVB is most likely to be successful with acute guttate and thin plaque psoriasis, especially if there is a history of improvement on exposure to sunlight. It is less likely to be successful with very thick plaques, especially if there is a dense surface scale.

Extensive psoriasis prior to NB-UVB

Psoriasis has cleared after 22 treatments
An increasing range of skin diseases is reported to clear or improve with NB-UVB but these respond less predictably and may require a greater number of treatments.
The mechanism of action of UVB on various skin diseases but is probably related to the suppression of major components of cell-mediated immune function.
UVB results in erythema, which begins 2–6 hours after exposure, peaks at 12–18 hours after exposure and generally persists for 48 hours.
Patient safety is paramount as overdose can result in severe and potentially life-threatening burns.


Individual skin response to UVB depends on skin phototype, prior exposure to sunlight or another source of UV and the presence of photosensitivity. Skin phototypes are determined by carefully questioning the patient but may be assigned incorrectly.
For BB-UVB therapy it is useful to measure Minimal Erythema Dose (MED) in skin types 1 to 4. There is a very wide range of MEDs within each skin type and a substantial degree of overlap in the MED values among different skin types.
MED is typically measured as follows.

MED testing template
MED testing
Recommended BB-UVB MED test doses (mJ/cm2):
| Skin Type | Square 1 | Square 2 | Square 3 | Square 4 | Square 5 |
|---|---|---|---|---|---|
| 1 | 10 | 20 | 30 | 40 | 50 |
| 2 | 20 | 30 | 40 | 50 | 60 |
| 3 | 30 | 40 | 50 | 60 | 70 |
| 4 | 40 | 50 | 60 | 70 | 80 |
MED is rarely measured in phototherapy departments in New Zealand. The test is somewhat inconvenient and difficult to perform accurately. NB-UVB is only available as 6-foot TL-01 bulbs, which are impractical for testing.
The manufacturer of the equipment may provide recommended starting doses. This may be a standard dose for all patients or may depend on skin phototype or measured MED. Most patients attend three times weekly. Twice weekly is less effective and once weekly is ineffective. Inpatients may be treated five times weekly but this is rarely practicable or tolerated by outpatients. Clearance generally occurs with the same total number of treatments if UVB is delivered three, four or five times weekly.
Patients should receive increasing doses each visit until erythema develops or until a prescribed maximum dose has been reached. The maximum depends on phototype and local protocol.
For most patients, the whole body is treated except the face and genitals.
Typically, the first treatment is 70% MED when known. It is more cautious for photodermatoses. The time to deliver the total dose will depend on the energy output of the source/irradiance.
Here is a typical chart that uses estimated skin phototypes to determine the initial dose and subsequent increments each treatment, in the absence of erythema.
Recommended BB-UVB doses (mJ/cm2):
| Skin type | Initial dose | Subsequent increase |
|---|---|---|
| 1 | 21 | 10% |
| 2 | 35 | 10-15% |
| 3 | 49 | 15% |
| 4 | 63 | 15-20% |
| 5 | 84 | 20% |
| 6 | 105 | 20% |
Usually, a standard starting dose of 50–100 (mJ/cm2) is used with increments 10–40% per treatment depending on skin phototype.
The development of significant erythema precludes further dose increments. Although undesirable, it is a necessary part of treatment for many patients in order to deliver the most effective dose to clear their skin disease. Suberythemal doses of NB-UVB are however effective in clearing psoriasis.

NBUVB burns

NBUVB blisters
The patient should be examined prior to each treatment. Erythema may be localised or generalised. Localised erythema can be protected allowing incremental exposures to the rest of the body, as scheduled, but generalised erythema should result in changes to the schedule.
Phototherapy staff should inform the physician if significant symptomatic erythema arises.
If treatment is interrupted, doses may need to be reduced to the starting dose or as follows:
One week: hold at previous dose
2 weeks: reduce dose by 25%
3 weeks: reduce dose by 50%
4 weeks or more: restart schedule
Interruptions to treatment are the most common reason for the failure of phototherapy. Tanning/keratinocyte hyperplasia may reduce the penetration of UVA, but lack of tanning could result in symptomatic erythema.
A course is completed when the skin disease has cleared more than 90% compared to baseline, or according to a pre-determined maximum number of treatments, commonly 40. Maintenance therapy is not generally recommended (except perhaps for cutaneous T-cell lymphoma).
Other treatment options should be considered in patients who fail to clear or substantially improve with UVB phototherapy. Plaques of psoriasis should be thinning by 12 treatments and by 30 treatments psoriasis should be 75% improved or better.
Phototherapy may be recommenced on relapse, depending on the severity of the disease, other treatment options and individual factors.
Some areas of skin disease may prove more resistant to UVB than others, often because of prior sun exposure. Commonly, in patients with psoriasis, additional UVB is delivered to the lower limbs. After the whole-body dose has been given, the patient dresses up to protect the rest of the body from further exposure. An extra 50% of the day's dose is delivered to the resistant sites.
Many patients are treated with additional topical or systemic therapy. In some cases, the additive benefit has been demonstrated by clinical trials. For example, adding emollients, coal tar ointment or calcipotriol ointment and/or oral acitretin or methotrexate can reduce the number of UVB treatments required to clear psoriasis. In atopic dermatitis, it may be advantageous to add in UVA as well as topical steroids, emollients and when necessary, oral antibiotics.
Emollients applied to scaly skin immediately before exposure to UVB must not act as sunscreens. Paraffin and coconut oil are satisfactory. Peanut oil should be avoided because of the risk of anaphylaxis.
Acute complications include:
Long-term complications include:
A total-body phototherapy unit should include safety features such as proper electrical grounding, accurate dosimetry device, protective shielding of the lamps, handrails for support, viewing window for staff observation, doors that open easily and adequate cooling.
Equipment used to treat patients must comply with New Zealand's stringent electrical regulations.
Phototherapy staff should keep records documenting each patient's treatment including exposure dose, the area treated, extent/severity of disease and degree of erythema. Some units are able to record this information automatically but a hard copy backup is recommended. Treatments that were withheld should be recorded with the reason for it. Record the follow-up arrangements during the course of treatment and after it has been completed.
Records may include:
The excimer laser emits radiation at 308 nm and can be used to treat localised plaques of psoriasis. Typically the laser is used three times a week and achieves 90% clearing of plaques in an average of 10 treatments, i.e. more rapidly than other forms of phototherapy. Typically a spot size of 3.5 cm is used at 2 minimal erythema doses and a pulse width of 30 ns. Common side effects include erythema, blisters, hyperpigmentation, and erosions, but they are well tolerated. Excimer laser treatment spares uninvolved skin. Remission rates are similar to narrowband phototherapy.
This treatment is not yet available in New Zealand. However, other forms of targeted UV are available at certain dermatologists' offices including Daavlin T500x.
Compare and contrast narrowband UVB machines from different manufacturers.
Information for patients