Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Demodex — extra information
Introduction Demographics Clinical features Diagnosis Treatment
What is demodex?
Demodex is the name given to tiny mites that live in the hair follicle. In humans, demodex is found on facial skin, especially the forehead, cheeks, sides of the nose, eyelashes and external ear canals. It sometimes causes a condition called demodicosis.
There are two mites principally involved in human demodex infestations, Demodex folliculorum and Demodex brevis. D. folliculorum is found in small hair follicles, particularly the eyelashes. In both its immature and adult stages, it feeds on skin cells. D. brevis is found in the oil glands that are connected to small hair follicles and feeds on the gland cells.
The D. folliculorum mite is 0.3–0.4 mm in length and the D. brevis mite is 0.15–0.2 mm. They are almost invisible to the naked eye, but under the microscope, their structure is visible. The eight legs of this mite move at a rate of 8–16 mm/h, and this is mainly done during the night as bright light causes the mite to recede into the follicle.
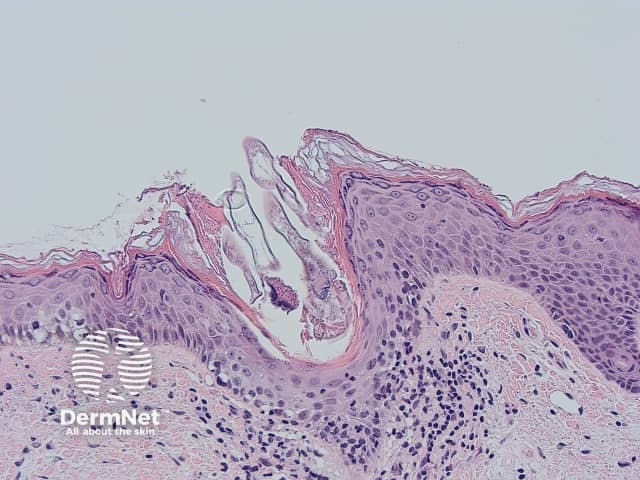
Demodex mite histology x200
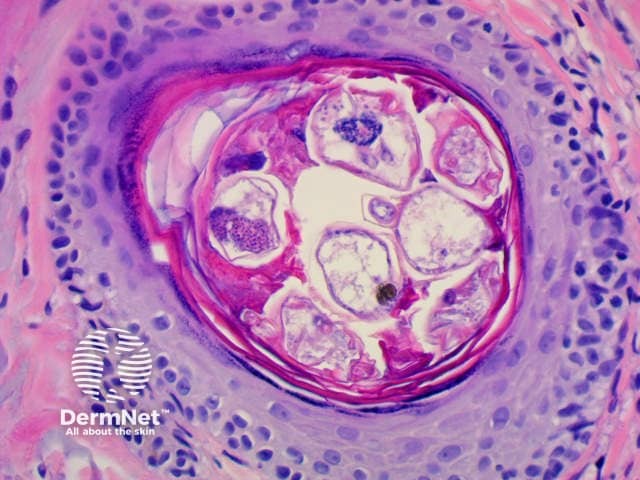
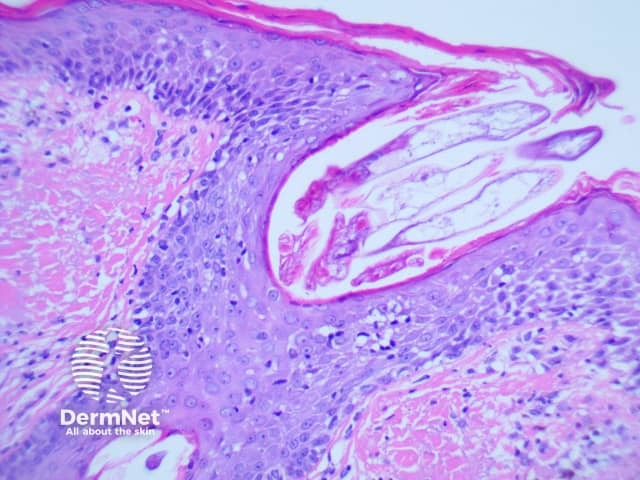
Demodex mite histology x400
Who has demodex and demodicosis?
Human demodex mites are a normal finding in older children and adults and are rarely observed in children under five years of age. Demodicosis is usually diagnosed in older adults, or immunodeficiency states, such as human immunodeficiency virus (HIV) infection.
What are the clinical features of demodicosis?
Demodicosis results in non-specific symptoms and signs on facial skin. These most often include:
- Follicular scales
- Redness
- Sensitive skin
- Itch.
Macules, papules, eczema, folliculitis and pigmentation have also been described.
Patients with demodicosis may have eye irritation, itching and scaling of eyelids (blepharitis or eyelid dermatitis). There may be lid thickening, loss of lashes (madarosis), conjunctival inflammation and decreased vision.
Increased numbers of Demodex mites have been observed in the following conditions:
- Demodex folliculorum – rough skin due to increased scale within hair follicles
- Demodectic frost of the ear – frosted, gritty follicular scaling of the ear lobe and helix
- Rosacea, particularly asymmetrical papulopustular or granulomatous variants
- Some cases of perioral dermatitis (also affecting periorbital or periauricular sites)
- Otitis externa (auricular demodex)
- Demodex abscess

Demodicosis

Rosacea due to demodicosis
Demodex folliculorum
The skin condition known as demodex folliculorum is also known as pityriasis folliculorum or spinulate demodicosis. It is a form of digitate keratosis, with slight redness and sandpaper-like texture of the skin due to follicular scale. It can cause irritation and burning sensation.
How is demodex diagnosed?
Dermoscopy typically shows spiky white structures occluding follicular openings.
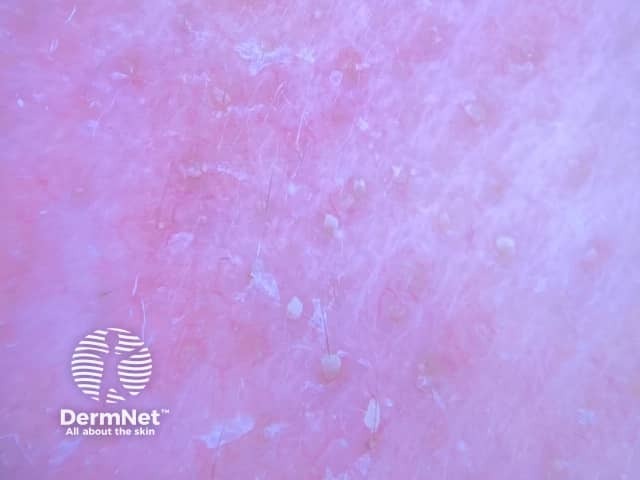
Dermoscopy of demodicosis
Demodex may be found in mineral oil skin scrapings from the face by KOH examination, or in hair follicles in a skin biopsy examined under the microscope. The superficial part of the horny layer of the skin and the follicular content can also be sampled by skin surface biopsy. Demodicosis is diagnosed when there is a high density of demodex mites (> 5/cm2).
Demodex folliculorum is characterised histologically by:
- Numerous demodex mites in the infundibula of the follicles
- Follicular hyperkeratosis
- Focal follicular lichenoid lymphocytic infiltrate
What is the treatment for demodicosis?
Demodex can only live in the human hair follicle, and when kept in check, they cause no problems. Home treatment and prevention strategies include:
- Using mild shampoo on hair and eyelashes every day
- Cleansing the face twice daily with a non-soap cleanser
- Avoiding oil-based cleansers and greasy makeup
- Exfoliating periodically to remove dead skin cells.
Treatment with acaricides is aimed at reducing the excessive proliferation of the mites, and by the clinical cure of symptoms and signs. Options include:
- Benzyl benzoate solution
- Permethrin cream
- Sulfur ointment
- Crotamiton cream
- Selenium sulfide wash
- Metronidazole gel
- Salicylic acid cream
- Ivermectin cream.
In severe cases, such as those with HIV infection, oral ivermectin may be recommended.
Periorbital demodicosis
Many treatments for periorbital demodicosis involve spreading an ointment at the base of the eyelashes at night to trap mites as they emerge from their burrow and move from one hair follicle to another. One treatment is to scrub the lashes and lash roots with baby shampoo, and then treat the area with tea tree oil or macadamia nut oil to try and kill any eggs.
References
- Book: Textbook of Dermatology. Ed Rook A, Wilkinson DS, Ebling FJB, Champion RH, Burton JL. Fourth edition. Blackwell Scientific Publications.
- Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, Sass U, Stene JJ, Thibaut S, Tytgat M, Seys B. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005 Jan;52(1):74–87. Medline
- Wallace MM, Guffey DJ, Wilson BB. Demodectic Frost of the Ear. JAMA Dermatol. Published online December 28, 2016. doi:10.1001/jamadermatol.2016.4769. Journal
- Forton FM, De Maertelaer V. Two Consecutive Standardized Skin Surface Biopsies: An Improved Sampling Method to Evaluate Demodex Density as a Diagnostic Tool for Rosacea and Demodicosis. Acta Derm Venereol. 2016 Aug 30. doi: 10.2340/00015555-2528. [Epub ahead of print] PubMed PMID: 27573185. Journal
On DermNet
Other websites
- Demodicosis – Medscape Reference
- Dermodecidosis – Therapeutics in Dermatology
- Two consecutive standardized skin surface biopsies – Youtube video (see Forton FM reference, above)
