Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Vanessa Ngan, Staff Writer; Copy Editor: Clare Morrison; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, October 2013. About Melanoma is sponsored by the New Zealand Dermatological Society Incorporated.
Introduction
Diagnosing spread of melanoma
Melanoma in the lymph nodes
Other tests
The only way your doctor can confirm whether or not your suspicious looking mole or spot is a melanoma is by cutting it out and sending it to a pathology laboratory for examination under a microscope.
If you have a suspected melanoma, your doctor will do a diagnostic excision (a type of skin biopsy). This usually means completely cutting out the tumour along with a 2 to 3-mm surrounding margin of unaffected skin to make sure that all the abnormal cells are removed. If your doctor is unsure of the diagnosis, suspects a thick melanoma or the tumour is located in a difficult site, you will be referred to a melanoma specialist who will be able to cut it out.
The excision skin sample will be sent to a pathology laboratory where it will be examined under a microscope by a pathologist (a doctor who is specially trained to diagnose disease by examining tissue). The pathologist can usually quickly confirm if you have a melanoma or other type of skin cancer. Sometimes the tissue sample undergoes extra tests to help with diagnosis. The tissue may be sent to other pathologists for their opinions.
You should get news of your biopsy results within 5 to 10 working days of having the tumour removed. If you have a melanoma, you may need to go back to your doctor for a wider excision to make sure that the entire tumour was removed along with a clear margin of normal tissue around the melanoma.

Trolley prepared for surgery

Putting in the local anaesthetic

Dressing applied to wound
Specimen pot
The pathologist’s report should include a macroscopic (as seen by the naked eye) and microscopic description of the tumour. The report will describe some or all of the following points:
If the tumour is confirmed as a melanoma, all the information in the pathology report will help in determining your prognosis (the likely course and outcome of your condition) and the risk of a new melanoma developing or of the original melanoma recurring.
Your doctor will examine you carefully, and will feel the local lymph nodes to see if they are enlarged.
If swollen lymph nodes are found, you may have an ultrasound scan for confirmation. Some cells may be removed from the lymph nodes by fine-needle aspiration (FNA).
If the glands are not enlarged, they may do a test known as a sentinel lymph node biopsy.
A milky fluid called lymph circulates through lymphatic vessels in the skin and drains to regional lymph nodes. These are found in your armpits, around the neck, in the groin and internally.
A sentinel lymph node is the very first lymph node where lymph from the melanoma is likely to drain, and may collect cancer cells from a deeply invasive tumour.
Sentinel node biopsy (SNB) involves taking a part of or removing a single lymph node, which is then examined under a microscope. To find this lymph node, the melanoma surgeon injects a blue dye into the site of the melanoma. A radioactive tracer is often used as well. Sentinel lymph node biopsy is not necessary for thin invasive melanoma or for in-situ melanoma (where melanoma is only found in the top layer of skin).
Swollen lymph nodes |
Looking for SNB |
Dye seen in lymph node during SNB |
Dye remaining in skin after SNB |
|---|---|---|---|

|
 Looking for sentinel node |
 Dye seen in lymph node during sentinel node biopsy |
 Sentinel node biopsy persistent tattoo |
If the results of ultrasound scan, FNA or SNB are positive for melanoma, you may need further surgery to remove all the lymph nodes in the area. If no cancer cells are found, the melanoma is unlikely to have spread to other areas (although this may rarely occur).
When melanoma has spread to your lymph nodes, the node usually forms a firm to hard lump. If this occurs between planned follow-up visits, you should let your doctor know immediately.
Most people who have had a melanoma removed do not need any other tests. However, if the doctor is suspicious that the melanoma may have spread to other areas or metastasised, a PET-CT scan may be arranged.
A PET-CT scan is a useful imaging test that can help tell if any lymph nodes are enlarged or if melanoma has spread to other organs in the body. Depending on where you get the test done, you may have to undergo a separate CT (computed tomography) scan and a separate PET (positron emission tomography) scan. Some imaging centres may have newer machines that can do a PET and CT scan at the same time.
A CT scanner rotates around you while you lie on a table, and takes cross-sectional images of your body. Before the scan you may need to drink or have injected into you a contrast dye that helps to show up any unusual areas in the body. The CT scan can pick up abnormalities in soft tissues so it is useful for finding enlarged lymph nodes or tumours on organs such as the lungs or liver.
In some cases, CT scans can be used to help guide a biopsy needle into a tumour that has grown inside the body. A radiologist moves a biopsy needle through the skin, toward the tumour and takes a needle biopsy sample. This is removed and looked at under a microscope by a pathologist.
In a PET scan you are injected with a radioactive substance that is taken up by cancer cells. After about an hour you will lie down on a table while the PET scanner takes pictures of areas of radioactivity in your body. This will show up areas where cancer might have spread to around your whole body.
With machines that can do both a PET and CT scan at the same time, the PET scan can highlight areas where the cancer may have spread to and then the CT scan can provide more detailed information about the spread.
CT scan: brain metastasis |
PET-CT scan: liver metastasis |
PET-CT scan: metastasis glows in groin |
|---|---|---|
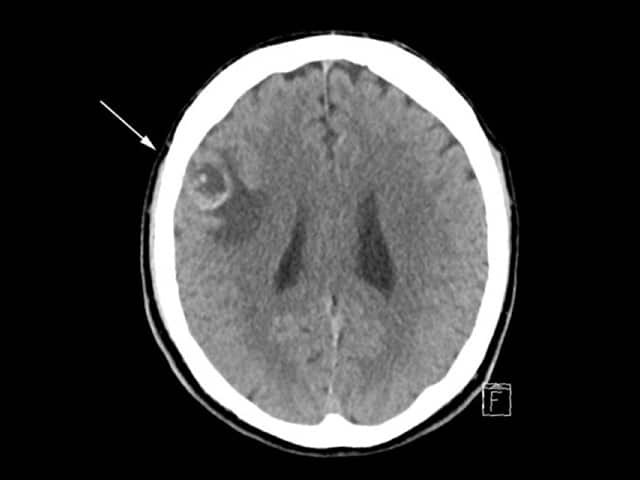 CT scan of brain with melanoma metastasis |
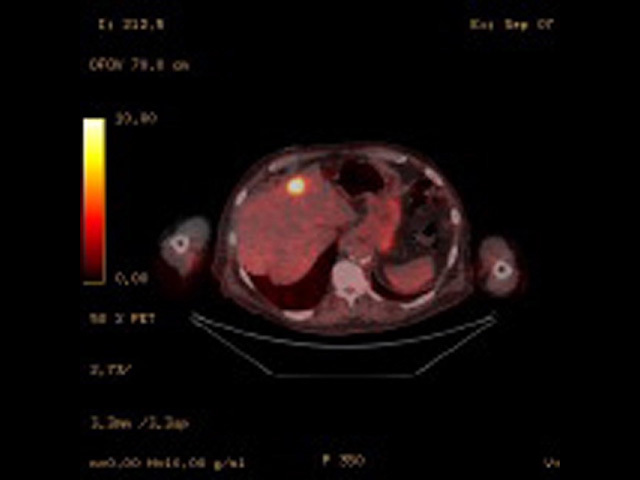 Fused PET/CT image of liver metastasis |
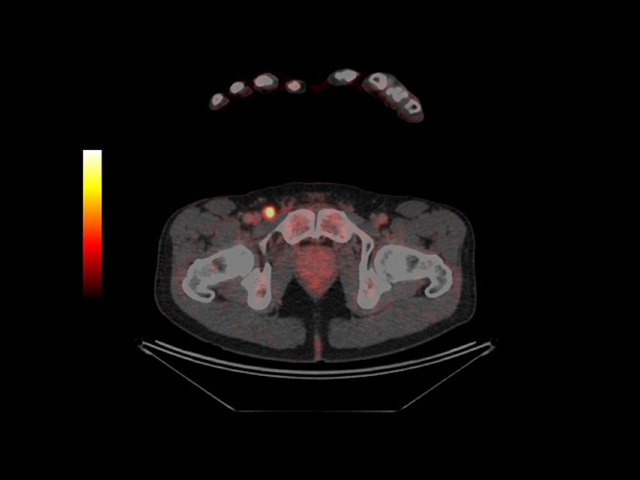 PET-CT scan revealing metastatic melanoma in groin |
Other tests you may need to have include:
Previous: See your doctor.
Next: Pathological diagnosis.
Melanoma: investigations and oncology referral video (Dr Lydia Chan).