Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Richa Tripathi, Consultant Dermatologist, Grande International Hospital, Kathmandu, Nepal. Copy edited by Gus Mitchell. November 2021
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
Non-dermatophyte mould onychomycosis (NDMO) is an opportunistic fungal nail infection (onychomycosis) caused by moulds.
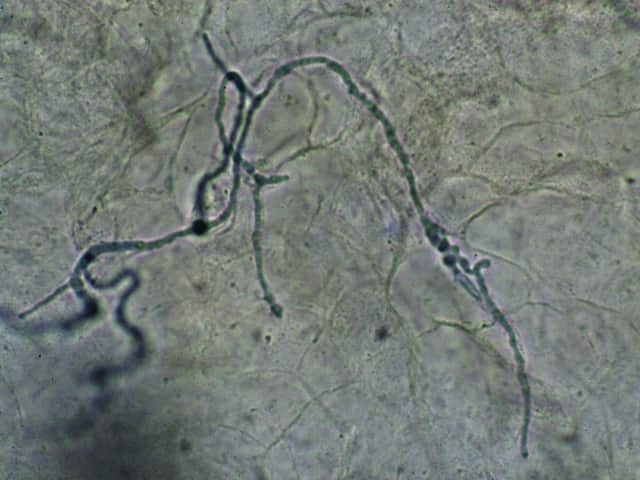
Moulds are ubiquitous in the environment, and thus are common contaminants that grow in nail fungal culture. Most moulds are non-keratolytic (except for Neoscytalidium dimidiatum) and require the presence of underlying trauma or other nail disease to penetrate the nail.

Aspergillus infection

Fusarium infection

Fusarium infection
Non-dermatophyte mould onychomycosis constitutes approximately 10% of onychomycosis cases globally. Recent reports suggest a rise in prevalence, especially cases presenting with a dermatophyte co-infection.
Risk factors identified for NDMO are similar to those for onychomycosis as a whole.
Risk factors include:
Different moulds have been identified as causing onychomycosis based on the geographical region. The most common species reported are:
Non-dermatophyte mould onychomycosis most often only affects one nail; toe nail involvement is 25 times more common than fingernail involvement.
The clinical sub-types of non-dermatophyte mould onychomycosis are similar to dermatophyte nail infections and include:
Paronychia is often present.
Infection may also lead to various nail colour changes depending on the infecting species. For example, infection with Aspergillus niger typically results in a black nail colour.
As most moulds require the presence of an underlying nail condition to penetrate the nail, definitive diagnosis can be challenging.
The following diagnostic criterion has been established and the presence of 3 or more of the following criteria confirms diagnosis:
Recent diagnostic advances for non-dermatophyte onychomycosis include molecular diagnostics using PCR technology.
See also laboratory tests for fungal infections and dermatological investigations and tests.
Hendersonula infection
Mould infections are more difficult to clear than dermatophyte infections and may require a combination of topical and oral therapies to clear the fungal infection.
Non-dermatophyte mould onychomycosis often requires a longer duration of treatment compared to treatment for dermatophyte nail infection. The possibility of relapse is also higher.