Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
Note: dermoscopic images in this course are nearly all at the same magnification; the full width of the image is equivalent to 12 millimetres on the patient.
Exogenous pigmentation Nail pigmentation due to trauma Pseudomonas infection Dermatophyte infection 



The nail plate is a semi-transparent keratinous structure and is not normally pigmented. It may appear discoloured because of pigment on top of the nail plate, within the nail plate or on top of the nail bed. Pigment may arise from the distal or proximal nail matrix.
Longitudinal melanonychia is due to activation of melanocytes in the nail matrix. It is more common in darker skinned individuals and may affect one or several nails. The band may occasionally extend across the entire nail (total melanonychia). Transverse melanonychia is rare.
There are various causes of longitudinal melanonychia.
Nails grow slowly, taking months to reach the distal edge, and longitudinal melanonychia reflects melanin deposition rather than the site of its production.
Melanonychia may be confused with discolouration due to blood spots. However, blood spots may also be seen in melanoma.
Nail seen from above Nail seen end-on 

To improve the quality of the dermoscopic image, apply gel to the nail. Examine the nail plate from above as well as end-on (the free edge of the nail). Seen end-on:
Dermoscopy is mainly used to assess pigmented streaks or bands, which usually extend from the proximal nail fold adjacent to the cuticle to the distal edge. Several structures have been described.
Melanocytic naevus Melanocytic naevus Pseudo-Hutchinson sign 




Melanocytic naevus of the nail apparatus is characterised by:
Dark pigmented bands may result in the pseudo-Hutchinson sign, in which the pigmentation is visible through the transparent nail fold.
Lentigo 
Epithelial melanin results in ethnic-type pigmentation, lentigo, and drug-induced pigmentation. The resulting melanonychia is characterised by:
Benign melanonychia due to epithelial melanin may affect multiple nails, particularly in individuals with skin phototype 5 or 6. They are more often observed on fingernails than toenails. They may be seen as part of Laugier-Hunziker syndrome or Peutz-Jeghers syndrome.
Congenital melanocytic naevi of the nail matrix are uncommon but may appear alarming. Features may include:
Melanoma should be considered if pigmentation affects a single nail, especially if it is of recent origin in an adult. Thumb nail and great toenail are most often affected. Melanoma may affect the nail bed (subungual) or matrix (pigment within nail plate).
Dermoscopic features of nail matrix melanoma include:
These features are not entirely reliable and should not be used as a substitute for biopsy if there is any doubt about the origin of longitudinal melanonychia.
Dermoscopy of subungual melanoma Dermoscopy of subungual melanoma 

Nail bed melanoma or subungual melanoma results in a red, brown or black nodule under the nail plate, which ulcerates and bleeds. It may resemble pyogenic granuloma.
Dermoscopy of subungual haemorrhage Dermoscopy of subungual haemorrhage Dermoscopy of subungual haemorrhage Dermoscopy of subungual haemorrhage 
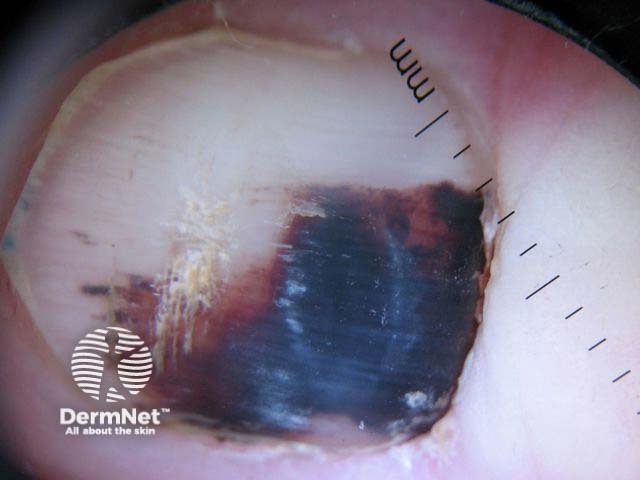


Subungual haemorrhage is the most common cause for pigmentation of the nail; patients often deny trauma and may be unable to give a clear history. The presence of red to bluish-black blood spots on dermoscopy is helpful.
Blood spots are well-circumscribed dots, globules or blotches; they may be red, purple, blue, brown or black. The proximal edge tends to be rounded and well circumscribed, whereas the distal edge is more likely to show parallel linear structures.
Blood spots sometimes grow out more slowly than the nail because they are under the nail plate rather than incorporated within it. Treat recurrent haemorrhage with suspicion; a tumour may be responsible.
Squamous cell carcinoma in situ Keratoacanthoma Amelanotic melanoma Glomus tumour 



Tumours of the nail unit may be nonpigmented, when diagnosis is frequently delayed. They include benign and malignant lesions.
Dermoscopic features to be evaluated include:
What are the indications for nail biopsy? [See Braun et al's article below.]
References