Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
An objective dermoscopy report may be issued for each lesion of concern, and is particularly necessary when the dermoscopy is not performed by the patient's usual primary health practitioner or dermatologist.
A standardised way of reporting dermoscopic findings was described at the 1st World Congress of the International Dermoscopy Society (IDS) in May 2006. A consensus document produced by the Board of the IDS is to be published in the Journal of the American Academy of Dermatology during 2006. It includes ten points, categorised as either recommended or optional.
A lesion of concern may be identified by the patient, a family member, a health professional or an expert dermoscopist. Reasons the patient may be concerned about the lesion may include:
Clinical concern relating to melanoma may arise because of:
Alternatively, non-melanoma skin cancer may be present.
Dermoscopic concern may arise because of:
Lesions with the typical clinical and/or dermoscopic characteristics of melanoma should be excised with a 2-mm margin and the specimen sent for pathology. To guide the pathologist to evaluate a small area that is of concern, orientate the specimen using edge incisions, sutures or ink, and draw a map on the request form. Alternatively, make a superficial round incision using a 1 to 2-mm micropunch in the area of interest and leave the punch in place.
Atypical lesions that do not have diagnostic features for melanoma may also be excised for histology. Melanoma can arise from a naevus, but in about 70% of cases arises de novo. Initially de novo melanoma may lack diagnostic features of melanoma and may also lack features of naevi.
Whole body photographs and digital dermoscopic monitoring may be preferred for:
If no dermoscopic change is noted at 12 months, the lesion can be confidently diagnosed as a naevus.
The International Dermoscopy Society considers that dermatologists should aim to receive histology reports of 5 to 10 benign melanocytic lesions to every melanoma. Less than that should prompt more excisions, and more than 10 benign lesions to every melanoma should prompt more monitoring. However there are inevitably differences in individual practices, and lesions may be removed for reasons that do not directly relate to the risk of malignancy (e.g. cosmetic reasons or to relieve anxiety).
A dermoscopy report should include the following information:
MoleMap report 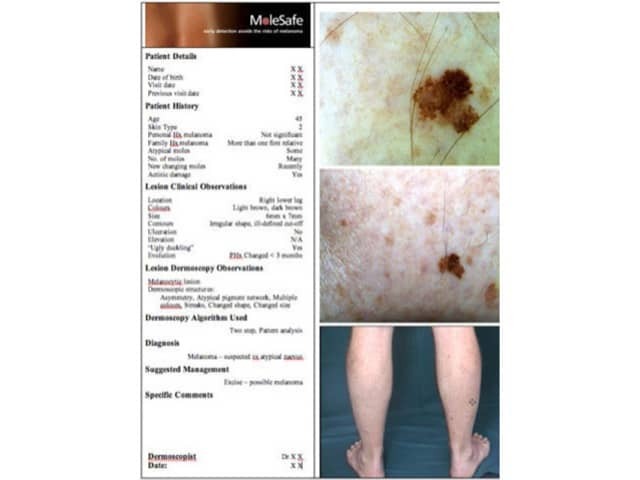
Compose a dermoscopy report for a lesion of concern.
Page 15 of 18. End of topics. Back to: Dermoscopy contents.
New topic – Melanocytic naevi: new classification
See the DermNet bookstore