Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Created 2008.
The first step algorithm identifies whether a lesion is melanocytic or nonmelanocytic. Various algorithms may be used to distinguish benign melanocytic lesions from malignant melanoma.
If these algorithms appear too complicated, use the 3-point checklist to identify malignant pigmented lesions.
The ABCD rule (Stolz method) is used for the dermatoscopic differentiation between benign melanocytic lesions and melanoma. The likelihood of melanoma depends on adding up the scores for different features as shown below.
| Criteria | Score X | Factor = | Results |
|---|---|---|---|
| Asymmetry In perpendicular axes: contour, colours and structures |
0–2 | 1.3 | 0–2.6 |
| Borders 8 segments: abrupt ending of pigment pattern |
0–8 | 0.1 | 0–0.8 |
| Colours White, red, light-brown (tan), dark-brown, blue-grey, black |
1–6 | 0.5 | 0.5–3.0 |
| Differential structural components or dermatoscopic structures (pigment network, structureless areas, dots, aggregated globules, branched streaks) | 1–5 | 0.5 | 0.5–2.5 |
| Total score | |||
| Benign | < 4.76 | ||
| Suspicious | > 4.76–5.45 | ||
| Melanoma | > 5.45 | ||
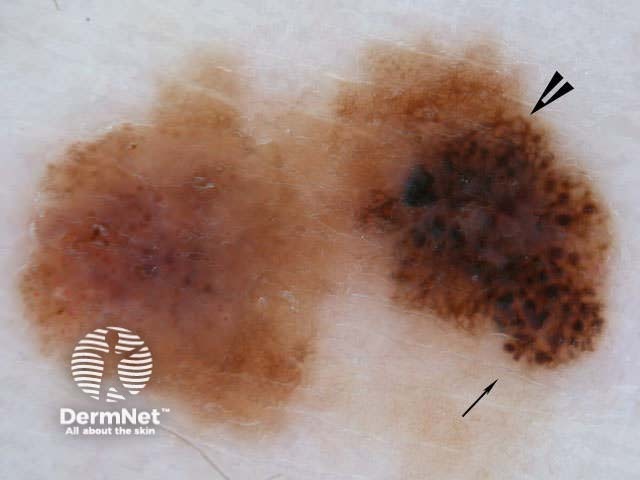
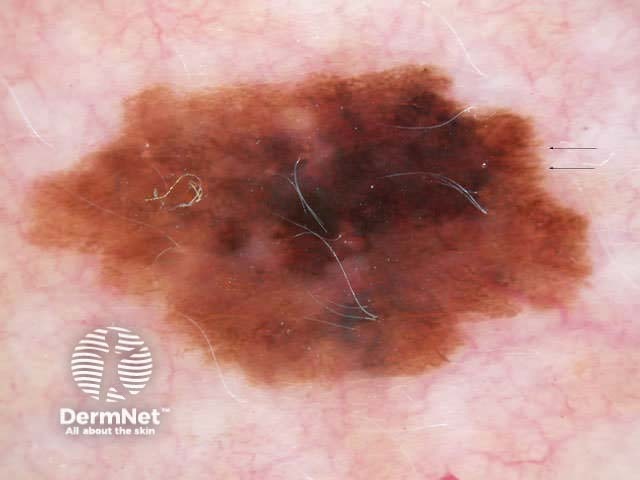
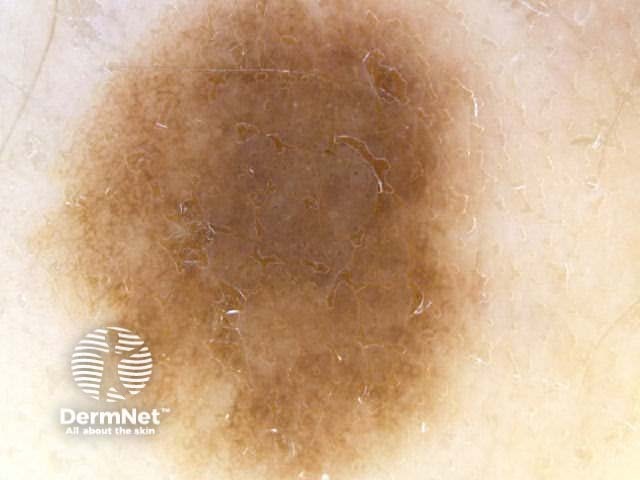
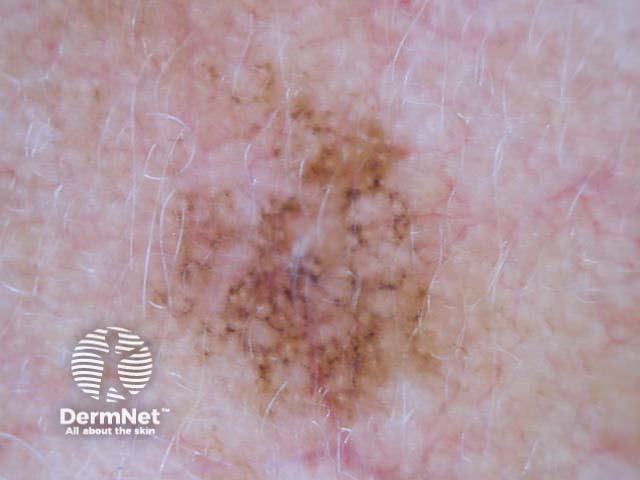
Asymmetry = 0 Asymmetry = 1 Asymmetry = 2 Borders = 0 Borders = 4 Borders = 8 Colours = 1 Colours = 3 Colours = 5 








Blum's modified ‘ABC-point list’ is simpler to use:
A – asymmetry of outer shape or differential structures inside the lesion in at least 1 axis
B – the abrupt cutoff of the network at the border in at least one-quarter of the circumference
C – 3 or more colours
D – 3 or more differential structures
E – noticed a change (evolution) in the last 3 months
Menzies method to distinguish the dermatoscopic features of benign melanocytic lesions from melanoma.
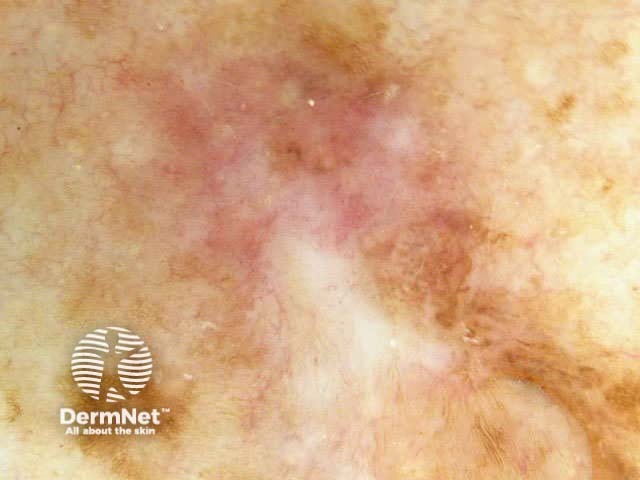
Negative features (benign lesions):
Symmetrical pattern Symmetrical pattern Single colour Single colour 



Positive features (melanoma):
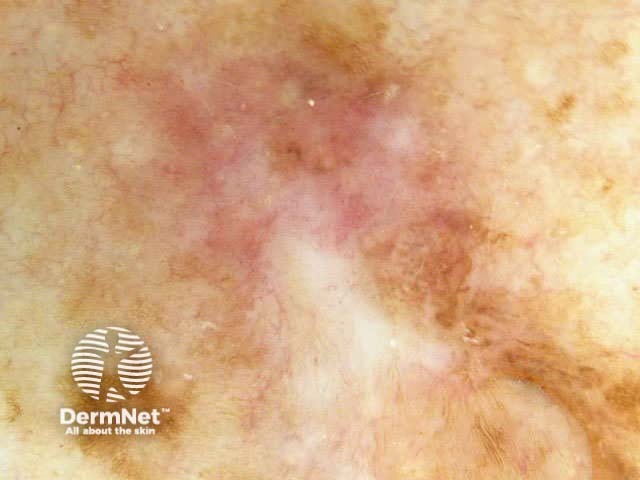
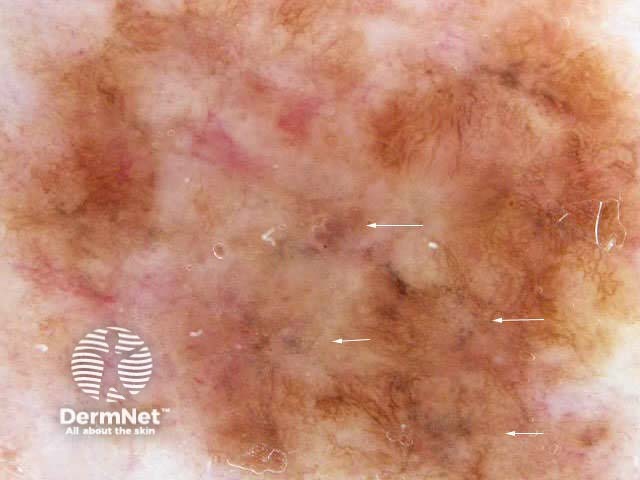
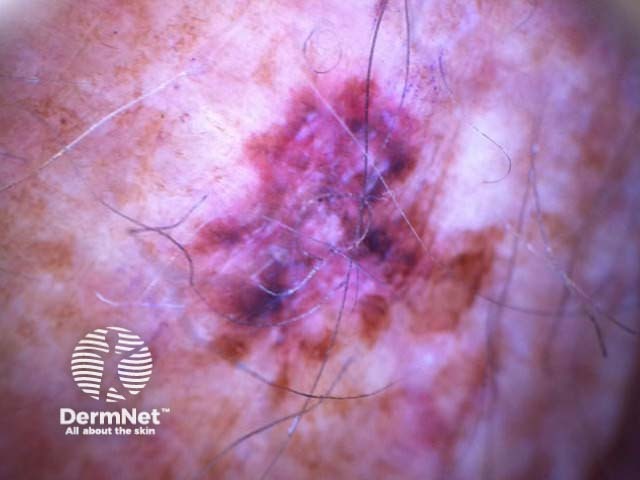
Blue-white veil Multiple brown dots Pseudopods Radial streaming Scar-like depigmentation Multiple colours (5) Multiple blue/grey dots Broadened network 




7-point checklist (Argenziano) for the dermoscopic differentiation between benign melanocytic lesions and melanoma (scores in brackets). The scores should be added up. Three or more indicates melanoma.
The seven-point rule has been revised (2011) so that each item scores 1 (total is 7). IN patients with atypical naevi, any lesion with a score of one should be carefully examined and excision of such lesions will pick up many early-stage melanomas.
Atypical pigment network Blue-whitish veil Atypical vascular pattern Irregular streaks Irregular dots/globules Irregular blotches Regression structures 




C.A.S.H. (Kopf et al) is used for the dermatoscopic differentiation between benign melanocytic lesions and melanoma (scores in brackets).
| Low | Medium | High | |
|---|---|---|---|
| Colours: few vs many Light brown, dark brown, black, red, white, blue Score 1 point for each colour |
1-2 colours (1-2 points) | 3-4 colours (3-4 points) | 5-6 colours (5-6 points) |
| Architecture: order vs disorder Score 0-2 points |
None or mild disorder (no points) | Moderate disorder (1 point) | Marked disorder (2 points) |
| Symmetry vs asymmetry Consider contour, colours and structures Score 0-2 points |
Symmetry in 2 axes (no points) | Symmetry in 1 axis (1 point) | No symmetry (2 points) |
| Homogeneity vs Heterogeneity Consider pigment network, dots/globules, blotches, regression, streaks, blue-white veil, polymorphous vessels Score 1 point for each structure |
Only one structure (1 point) | 2 types of structure (2 points) | 3 or more structures (3-7 points) |
Add up the scores for a total C.A.S.H. score (2 to 17).
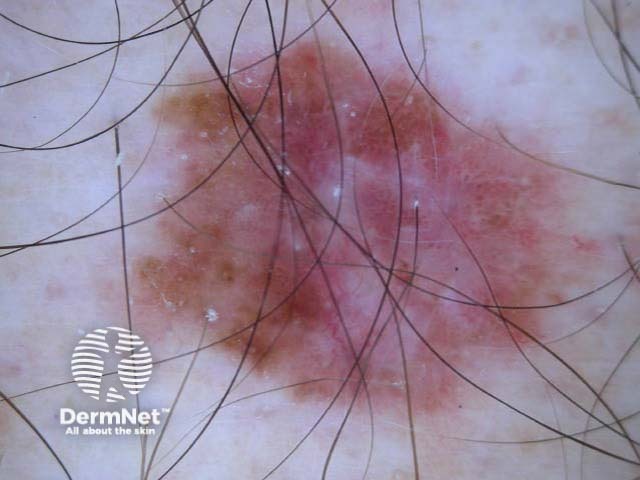
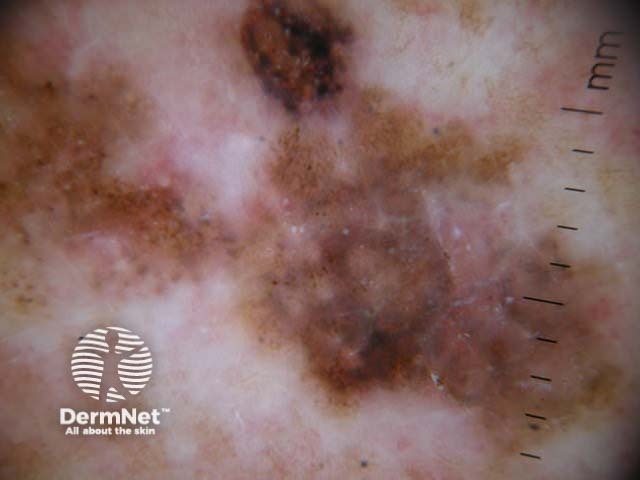
C=4, A=1, S=1, H=4. Total CASH score=10 C=4, A=2, S=2, H=5. Total CASH score=13 C=4, A=1, S=1, H=3. Total CASH score=9 C=3, A=1, S=2, H=3. Total CASH score=9 C=4, A=2, S=2, H=3. Total CASH score=11 C=4, A=2, S=2, H=4. Total CASH score=12 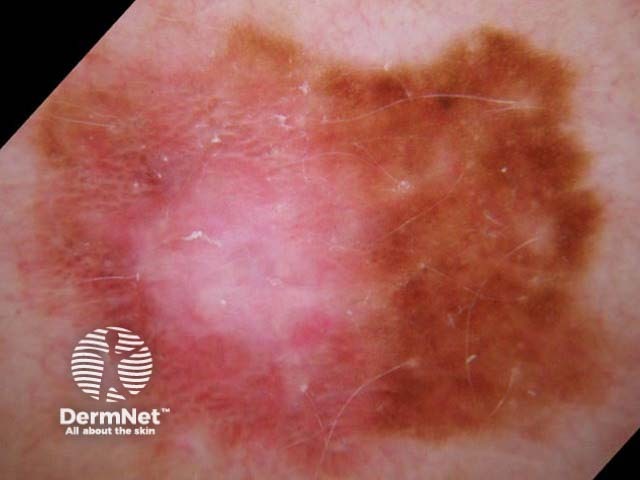




A modified form of pattern analysis (Kittler, Rosendahl et al) looks for CHAOS (asymmetry of structure and/or colour) and at least one clue to diagnose malignancy. It can be applied to melanocytic and nonmelanocytic lesions. This method does not use the 2-step rule.
Patterns are described by multiple elements of the same type: lines, dots, clods, circles, pseudopods (a line with a bulbous end) and structureless areas. Structureless areas are made up of colours: black, dark brown, light brown, grey, blue, orange, yellow, white, red and purple.
Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern Symmetrical dermoscopic pattern 






Asymmetrical patterns should lead to looking for specific clues to malignancy. The clues to malignancy (melanoma and nonmelanocytic tumours) are:
Chaos + eccentric structureless area, blue/grey structures, white lines, peripheral black dots Chaos + eccentric structureless area, polygons Chaos + eccentric structureless area, polymorphous vessels Chaos + blue/grey structures, polymorphous vessels Chaos + peripheral black dots, blue/grey structures, eccentric structureless area, white lines, poly Chaos + eccentric structureless area, peripheral black dots, polygons Chaos + thickened reticular network, eccentric structureless area Chaos + thickened reticular network, eccentric structureless area, polygons 





Some of these images are of poor quality, but the algorithm still works.
The BLINK algorithm has been devised to identify malignant lesions, particularly nodular melanoma, as this tumour often lacks conventional dermatoscopic features. It can also be used for nonmelanocytic lesions.
| Benign | If not, then consider the following: | |
| Lonely | An ugly duckling | Score 1 |
| Irregular | Asymmetrical pigmentation pattern or > 1 colour | Score 1 |
| Nervous | Nervous patient OR changing lesion | Score 1 |
| Known | Known clues to malignancy | Score 1 |
Clues to malignancy are:
A score of ≥2 requires a biopsy.
I=1, K=1 (atypical network, eccentric structureless zone) I=1, K=1 (segmental streaks, irregular black dots, eccentric structureless zone) I=1, K=1 (atypical network, irregular black dots, eccentric structureless zone) I=1, K=1 (atypical network, irregular black dots/clods) I=1, K=1 (atypical network, segmental streaks, eccentric structureless zone) I=1, K=1 (atypical network, eccentric structureless zone) 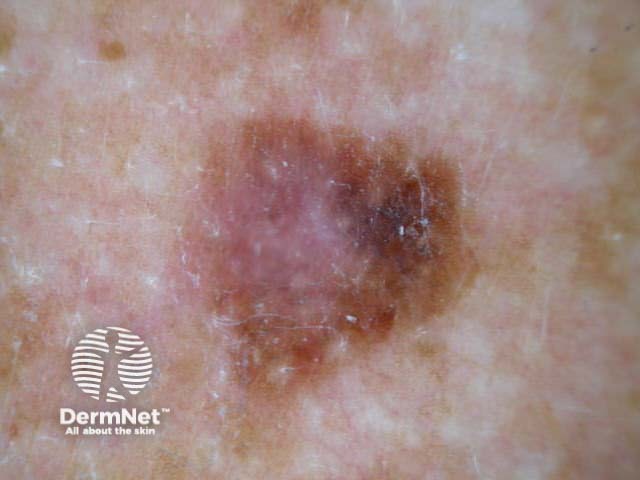




Some of these images are of poor quality, but the algorithm still works.
TADA is an acronym for Triage Amalgamated Dermoscopic Algorithm. TADA does not require a diagnosis to be made in order to decide if the lesion should be excised or referred to an expert. TADA is reported to have a sensitivity of 94.8% and specificity of 72.3% for malignant skin lesions.
The first step is to determine whether the lesion has features of:
If yes, exclude from further analysis. If no, is there any architectural disorder? If there is architectural disorder, does the lesion have one or more of the following 6 predictive factors?
If yes, consider excision or refer.
If no, the lesion is likely to be benign. Any doubt, follow-up or refer.
Find the evidence to support the use of the algorithms. Which is the best?
See the DermNet bookstore.