Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Diffuse alopecia — extra information
Diffuse alopecia
Author: Dr Harriet Bell, House Officer, Auckland City Hospital, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof. Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. October 2019.
Introduction Demographics Classification Excessive hair shedding Hair thinning Complications Diagnosis Treatment and outcome
What is diffuse alopecia?
Alopecia is the medical word meaning hair loss. Alopecia is diffuse if it affects the scalp in a general distribution. This is in contrast to localised or focal alopecia, which is characterised by patchy hair loss.
Who gets diffuse alopecia?
Diffuse alopecia is common, affecting up to 50% of men and women. While it can affect both sexes at any age, women present more frequently than men [1,2].
The hair cycle
Hair follicles cycle through growing and resting phases.
- Anagen (growth phase) lasts two to six years.
- Catagen is the short transitional phase, lasting four to six weeks.
- Telogen (resting phase) lasts two to three months and ends with the release of the hair from the follicle [3,4].
How is diffuse alopecia classified?
Diffuse alopecia can be categorised into conditions that cause excessive hair shedding and conditions that cause hair thinning [1].
Excessive hair shedding
Abnormal hair shedding (or effluvium) may occur during the telogen or anagen phase of the hair cycle.
Telogen effluvium
Telogen effluvium is the most common cause of diffuse hair shedding [3,5]. A triggering event causes an increased number of anagen hairs to prematurely enter the catagen and then telogen phase. Excessive shedding of telogen hairs occurs a few months after the triggering event [3].
Patients may notice clumps of hair falling out on their hairbrush or while showering [6]. Up to 30–50% of scalp hair may be lost [1]. The excess hair shedding may produce diffuse thinning, bitemporal recession, or expose a pattern hair loss in those genetically predisposed [3].
Many triggers have been implicated in telogen effluvium; these include:
- Severe illness or high fever
- Childbirth
- Iron deficiency
- Thyroid disease (hyperthyroidism or hypothyroidism)
- Kidney or liver disease
- Malnutrition or crash diets
- Infections such as syphilis
- Medications (see Drug-induced alopecia)
- Emotional stress
- Systemic lupus erythematosus [3,6].

Telogen effluvium

Telogen effluvium

Hair brushings during episode of telogen effluvium
Anagen effluvium
Anagen effluvium occurs when the anagen phase is interrupted, causing premature termination of hair growth and abrupt hair shedding.
Anagen effluvium is most commonly due to chemotherapy (see Drug-induced alopecia) and usually begins one to two weeks after treatment is started. It may result in 80–90% loss of body hair, including eyebrows and eyelashes [1,2]. It may also be caused by poisoning with thallium, colchicine or selenium [7].
Anagen effluvium may also be due to alopecia areata [2]. Alopecia areata is an autoimmune condition in those with genetic predisposition and usually presents as a patchy hair loss with bald patches (focal alopecia) [2,5]. Confluent or widespread alopecia areata presents with diffuse hair loss, sometimes resulting in complete baldness of the scalp (alopecia totalis) or total body hair loss (alopecia universalis) [1,2,5].

Alopecia areata

Alopecia totalis

Alopecia universalis
Hair thinning
Gradual diffuse hair thinning is due to male or female pattern hair loss [1,8].
Pattern hair loss
Male pattern hair loss is caused by a genetic predisposition that affects the sensitivity of hair follicles to circulating androgens; for this reason, it is sometimes called androgenetic alopecia [1,4]. The characteristic pattern is a bitemporal recession and balding at the vertex and frontal regions.
Female pattern hair loss has a strong genetic component, but the role of androgens is unclear [8]. The pattern is thinning over the top of the scalp with a widening of the midline part [1,4].
Pattern hair loss in females occurs earlier and more severely in polycystic ovary syndrome, with a virilising tumour, or on exposure to an exogenous androgen such as testosterone.

Female pattern alopecia
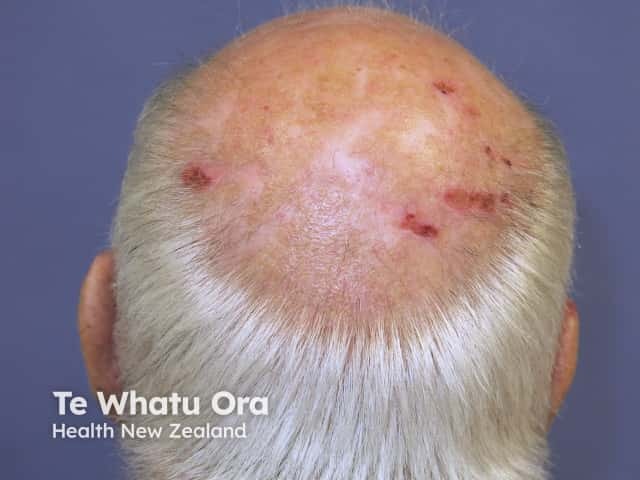
Male pattern alopecia

Female pattern alopecia. Credit Dr R Sinclair
What are the complications of diffuse alopecia?
Hair loss has minimal harmful physical effects; however, it may be psychologically damaging and negatively impact on the quality of life, as hair is linked with one’s identity (see Psychological effects of hair loss). Psychiatric disorders, including anxiety and depression, are more common in people with alopecia than in those without [6,9]. Loss of hair from the crown of the scalp often results in scalp trauma as scalp hair provides an early warning of impending contact.
How is diffuse alopecia diagnosed?
Diffuse alopecia is a clinical sign observed on examination. Additional tests may be used to diagnose the underlying cause [6].
History and examination
History may identify triggers or genetic susceptibility [6]. Women have been shown to accurately assess the percentage hair loss based on the change in the ponytail diameter or circumference.
Examination should include:
- Scalp examination should assess the degree and pattern of hair loss, and for signs of inflammation, redness, scaling, and scarring [2].
- The hair shaft length, diameter, and breakage should be assessed [2].
- Examination of the scalp with a dermatoscope (trichoscopy) may yield further information (see Dermoscopy) [4].
- Nail changes may be observed with diffuse alopecia (see Nail disorders).
- Beau lines are a groove in the nail coinciding with the time of the arrest in hair growth.
- Nail pitting is associated with alopecia areata [6].
Blood tests
Laboratory workup should be performed to identify treatable causes. This may include:
- Complete blood count and ferritin for anaemia and iron deficiency
- Thyroid function tests for thyroid disease
- Serum zinc level as zinc deficiency can be early evidence of coeliac disease
- Renal and liver function tests
- Antinuclear antibodies if features suggest systemic lupus erythematosus
- Hormonal evaluation (free androgen index, sex hormone-binding globulin, prolactin) in women with clinical signs of hyperandrogenism [2–4,8].
Hair pull test
The hair pull test involves grasping 40–60 closely grouped hairs and applying gentle traction. If more than 10% of hairs are easily pulled out, the test is positive [3].
- The hair pull test is positive in telogen effluvium, anagen effluvium, and diffuse alopecia areata [6].
- The hair pull test is negative (away from areas of hair loss) in male and female pattern hair loss [1].
Trichogram
For a trichogram, 20–50 hairs are plucked and examined under a microscope to estimate the percentages of anagen and telogen hairs.
- A normal result is >80% anagen hairs and <20% telogen hairs [4].
- Telogen effluvium is characterised by 25% telogen hairs [3].
- Exclamation point hairs (in which the hair shaft is narrower toward the scalp, mimicking an exclamation point) are typical of alopecia areata [6].
Scalp biopsy
To assess alopecia, two four-millimetre punch biopsies should be taken from the vertex of the scalp or where there are clinical signs [5]. It is important to clearly label the histology request form as being for investigation of alopecia so that one biopsy can be cut horizontally to determine the number of follicles.
- An increased number of telogen follicles (>15–25%) without inflammation is seen in telogen effluvium [3,5].
- A dense infiltrate of lymphocytes and other immune cells is seen in the deepest part of the hair follicles in alopecia areata [4].
- The miniaturisation of hair follicles (when the follicles produce progressively thinner hairs), and a low terminal hair to vellus hair ratio is seen in male/female pattern hair loss [2,8].
What are the treatment and outcome of diffuse alopecia?
The treatment and prognosis of diffuse alopecia depend on the underlying cause.
Telogen effluvium
Acute telogen effluvium resolves within three to six months and hair density returns to normal providing ongoing triggers or causative medications (see Drug-induced alopecia) have been identified and discontinued [5]. However if genetically predisposed, there may be a residual pattern alopecia. Treatment is not usually necessary [6].
Hair shedding that lasts longer than six months is known as chronic telogen effluvium. It tends to fluctuate over some years, then usually resolves spontaneously [5].
Anagen effluvium
Anagen effluvium is managed with observation and support [2].
- Scalp cooling may reduce chemotherapy-induced alopecia (see Skin toxicity of chemotherapy drugs) [10].
- Anagen effluvium usually resolves once chemotherapy is discontinued; permanent alopecia is rare [6].
Diffuse alopecia areata is challenging to treat. Even when treatment induces an increase in hair growth, hair loss may recur when treatment is stopped [1].
- For adults with less than 50% scalp involvement, treatment with intralesional corticosteroid injections may temporarily speed up regrowth [1,6].
- Short-term regrowth may be observed with topical corticosteroids, minoxidil, immunotherapy (eg, with diphenylcyclopropenone), and dithranol [1].
- Systemic corticosteroids can lead to regrowth, but the risks of long-term steroid use outweigh the benefits [1].
The natural course of diffuse alopecia areata is variable. One-third of patients recover spontaneously within six months, and 50–80% of these patients have persisting hair after a year. Some patients may have repeated episodes of diffuse alopecia areata [4,9].
The new hair that grows back may not be the same colour or texture as it was before it was lost [9].
The prognosis is worse for alopecia areata that is severe at its onset. Less than 10% of patients with alopecia totalis and alopecia universalis will recover [1].
Male and female pattern hair loss
Treatments for pattern alopecia should be continued indefinitely, as discontinuation results in recurring hair loss [4,6]. Treatments include:
- Topical minoxidil solution — it generally takes 6–12 months before improvement is observed [4,6]
- Oral finasteride — used for male pattern hair loss [4]
- Anti-androgen therapy for women includes oral spironolactone, cyproterone acetate, and finasteride, but there is limited evidence for efficacy [8].
Hairpieces and wigs, false eyelashes and eyebrows, and coloured sprays or make-up can be used to camouflage areas of balding.
Hair transplantation can be used to treat advanced male or female pattern hair loss [4].
References
- Mounsey A and Reed S. Diagnosing and treating hair loss. Am Fam Physician. 2009; 80: 356–62. PubMed
- Harrison S, Bergfeld W. Diffuse hair loss: Its triggers and management. Cleve Clin J Med. 2009; 76: 361–7. doi: 10.3949/ccjm.76a.08080. PubMed
- Malkud S. Telogen effluvium: A review. J Clin Diagn Res. 2015; 9: WE01–WE3. doi: 10.7860/JCDR/2015/15219.6492. PubMed Central
- Wolff H, Fischer TW, Blume-Peytavi U. The diagnosis and treatment of hair and scalp diseases. Dtsch Arztebl Int. 2016; 113: 377–86. doi:10.3238/arztebl.2016.0377. PubMed Central
- Sinclair R. Diffuse hair loss. Int J Dermatol. 1999; 38: 8–18. PubMed
- Phillips TG, Slomiany WP, Allision R. Hair loss: Common causes and treatment. Am Fam Physician. 2017; 96: 371–8. PubMed
- Yu V, Juhász M, Chiang A, Atanaskova Mesinkovska N. Alopecia and associated toxic agents: A systematic review. Skin Appendage Disord. 2018 Oct;4(4):245-260. doi: 10.1159/000485749. Epub 2018 Jan 5. Review. PubMed PMID: 30410891; PubMed Central PMCID: PMC6219226.
- van Zuuren EJ, Fedorowicz Z, Schoones J. Interventions for female pattern hair loss. Cochrane Database of Syst Rev. 2016; 2016: CD007628. doi: 10.1002/14651858.CD007628.pub4. PubMed Central
- Hunt N, McHale S. The psychological impact of alopecia. BMJ. 2005; 331: 951–3. doi: 10.1136/bmj.331.7522.951. PubMed
- Rugo HS, Voigt J. Scalp Hypothermia for preventing alopecia during chemotherapy. A systematic review and meta-analysis of randomized controlled trials. Clin Breast Cancer. 2018; 18: 19–28. doi: 10.1016/j.clbc.2017.07.012. PubMed
On DermNet
- Hair loss
- Telogen effluvium
- Alopecia areata
- Alopecia from drugs
- Female pattern hair loss
- Male pattern hair loss
- Psychological effects of hair loss
- Diseases of the hair and scalp
- False eyelashes and eyebrows
- Hairpieces and wigs
- Trichoscopy of generalised noncicatricial hair loss
