Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lesions (cancerous) Diagnosis and testing
Author: Naomi Ashman, Dermoscopist, Torbay Skin, Auckland, New Zealand. DermNet New Zealand Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. December 2018.
Introduction - lentigo maligna
Clinical features - lentigo maligna
Introduction - lentigo maligna melanoma
Clinical features - lentigo maligna melanoma
Dermoscopic features
Dermoscopic differential diagnosis
Histological explanation
Lentigo maligna is a type of melanoma in situ and is a precursor to lentigo maligna melanoma, a potentially serious form of skin cancer. Lentigo maligna is also known as Hutchinson melanotic freckle.
Lentigo maligna occurs in sun-damaged skin so is generally found on the bald scalp, face or neck, particularly the nose and cheek of older adults. It grows slowly in diameter over 5–20 years or longer.
Lentigo maligna presents as a slowly growing or changing patch of discoloured skin. At first, it often resembles a freckle or benign lentigo. It becomes more distinctive and atypical in time, often growing to several centimetres over several years or even decades. Like other flat forms of melanoma, it can be recognised by the ABCDE rule: Asymmetry, Border irregularity, Colour variation, large Diameter and Evolving.
The clinical characteristics of lentigo maligna include:
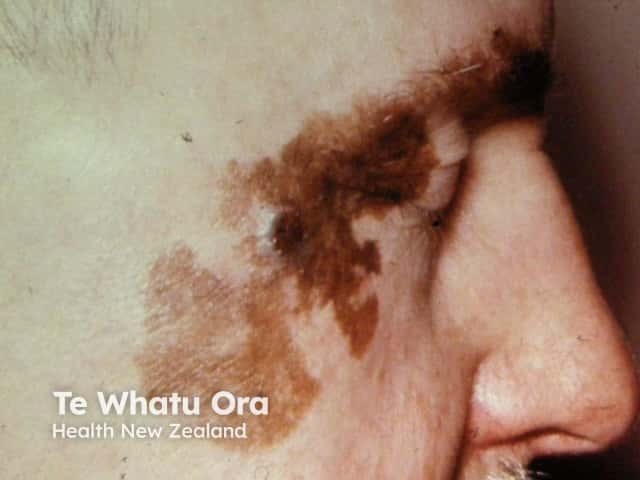
Lentigo maligna

Lentigo maligna

Lentigo maligna

Lentigo maligna

Lentigo maligna

Lentigo maligna
Lentigo maligna melanoma is diagnosed when the malignant melanoma cells have invaded into the dermis and deeper layers of skin. Lentigo maligna has a comparatively low rate of transformation to invasive melanoma (under 5%). The risk of invasive melanoma is greater in larger lesions, with up to 50% of those with a diameter of greater than 4 cm being reported to have an invasive focus.
Invasive melanoma is reported to arise within lentigo maligna in 3–10% of cases. The following features are very suspicious of invasion:

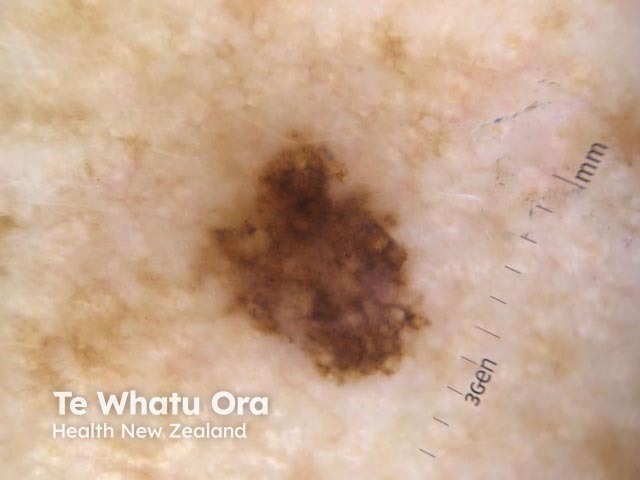
Lentigo maligna melanoma 0.8 mm

Lentigo maligna melanoma 0.98 mm

Lentigo maligna melanoma 1.7 mm

Lentigo maligna melanoma

Lentigo maligna melanoma

Lentigo maligna melanoma
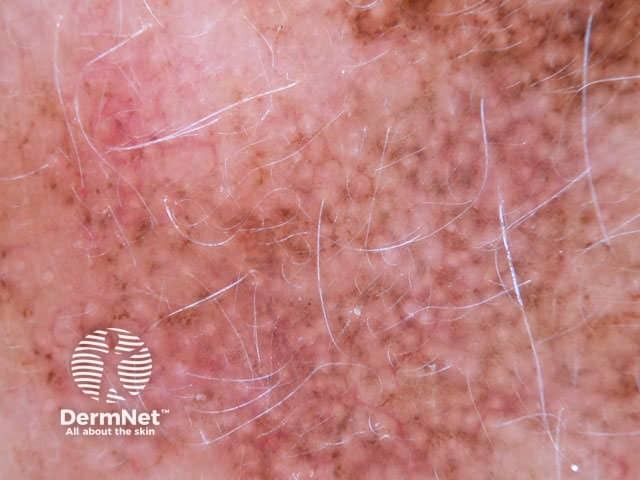
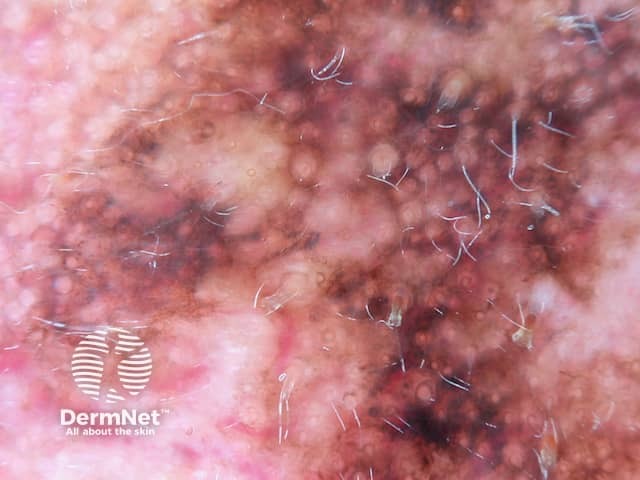
Annular granular pattern seen in dermoscopy of lentigo maligna
Annular granular pattern and rhomboids seen in dermoscopy of lentigo maligna
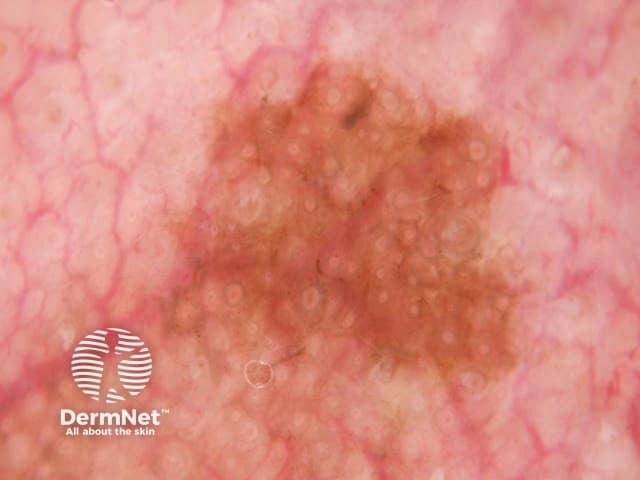
Grey concentric circles seen on dermoscopy of lentigo maligna
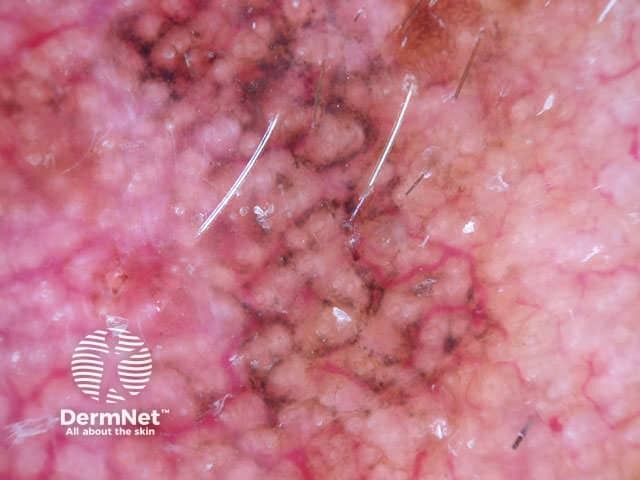
Lentigo maligna melanoma shows the dermoscopic features of lentigo maligna and of invasive melanoma.
In the absence of a pigment network, there may be amelanotic areas and irregular blotches.

Annular granular pattern and rhomboids seen in dermoscopy of lentigo maligna melanoma
Pseudonetwork, structureless areas, grey and concentric circles seen in dermoscopy of lentigo maligna melanoma

Perpendicular white lines and an irregular blotch with streaking seen in dermoscopy of lentigo maligna melanoma, Breslow 0.95 mm
The dermoscopic differential diagnosis of lentigo maligna and lentigo maligna melanoma includes:

Dermoscopy of seborrhoeic keratosis

Dermoscopy of solar lentigo

Dermoscopy of lichen planus like keratosis

Annular granular pattern seen in dermoscopy of pigmented actinic keratosis

Dermoscopy of a naevus on the face
Dermoscopy of superficial spreading melanoma
Lentigo maligna is a proliferation of malignant melanocytes along the basal layer of the epidermis and within the hair follicle.
Grey dots
Grey dots are formed by melanin in melanophages in the papillary dermis.
Asymmetrical pigmented follicular openings
Asymmetrical pigmented follicular openings are formed by melanophages within the hair follicle. Atypical melanocytes as single units or small nests extend along the circumference of the follicular epithelium.
Rhomboid structures
Rhomboid structures are created by the merging of asymmetrical pigmented follicular openings.
Structureless areas
Structureless areas are caused by the obliteration of the follicular openings.
Grey circles
Grey circles correspond to pigmented melanocytes within follicular infundibula. When melanophages are prominent, circles may appear to be comprised of grey dots.
Management of melanoma is evolving. For up to date recommendations, refer to Australian Cancer Council Clinical practice guidelines for the diagnosis and management of melanoma.