Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Jessica Rachel Maguire, IMT, Barts Health NHS Trust, London, United Kingdom, March 2022; updated by Dr Ian Coulson, Dermatologist, United Kingdom, April 2025.
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Scabies is a transmissible skin disease caused by the ectoparasitic mite Sarcoptes scabiei var. hominis. This variant infests humans only; scabies cannot be caught or transferred to other animals.
Scabies is a highly contagious infestation of the human epidermis. Scabies was described by Aristotle who likened the disease to ‘lice of the flesh’. Scabies presents as a rash with intense itching; it may have a characteristic appearance and distribution.
Scabies is a global disease, and anyone can be affected. It is estimated that about 204 million people are affected by scabies worldwide, with an annual incidence of 455 million cases. Scabies is more common in the elderly, children, and adolescents.
The burden of disease is higher in low-income areas, in the tropics, and in poorly resourced communities and countries.
Risk factors for scabies, particularly in developing countries, include:
In developed countries, scabies occurs in family outbreaks and children may acquire it from close play contact in school or sleepovers. In situations where there may be close physical contact for the delivery of personal care, such as in care homes, large outbreaks are not uncommon. In young adults, sexual spread is frequent.
Scabies infection is usually transmitted through close bodily skin contact such as holding hands for prolonged periods; spread amongst sexual partners is common. A brief handshake or hug does not usually allow for transmission unless the patient has crusted scabies.
Spread via fomites (clothing, towels, etc.) is very uncommon as the mite perishes within hours of leaving the host; it is relevant in crusted scabies.
Infection typically presents with a classical itchy rash. Lesions are symmetrical, and mainly affect the hands, wrists, axillae, thighs, buttocks, waist, soles of the feet, areola and vulva in females and penis and scrotum in males. The neck and above are usually spared, except in cases of crusted scabies and in infections occurring in infants, the elderly, and the immunocompromised.
However, the rash may be generalised and eczematous features may dominate and mask the classical signs. Clinical suspicion is paramount.

A scabies burrow on the toe

A burrow on the palm - the mite can just be seen adjacent to the vesicle

Numerous palmar scabies burrows in an elderly lady

Scabies burrows on the palm

Scabies burrows on a babies foot

Interdigital scaling in the first web space of the hand
This variant occurs in the elderly and immunosuppressed – the palms and soles become covered in crusted plaques. There is massive infestation with mites, numbering in the thousands; it is highly infectious and there may be heavy infestation of bedding and upholstery.

Thick crusted plaques on the thumb and palm due to crusted scabies in an elderly woman
This can be a widespread nonspecific eczematous eruption on the torso and limbs and may partially obliterate the primary pathognomonic features.
Scabies may present as granulomatous nodules in an infected person with a darker skin type.
Inflammatory changes appear as redness in white skin and greyness in black skin.
Other complications of classical scabies include:

Scabies with superadded streptococcal infection

Scabies nodules in the axilla

Axillary scabies nodules in an infant
A high index of suspicion should be used when assessing a patient with a new widespread itchy rash, especially one who reports itchy close contacts. The diagnosis is typically clinical and most easily confirmed using dermoscopy.
Several invasive and non-invasive tests exist to aid in confirming a diagnosis of scabies:
It is useful to examine close contacts in suspicious cases as pathognomonic signs are often seen in those with minimal symptoms.
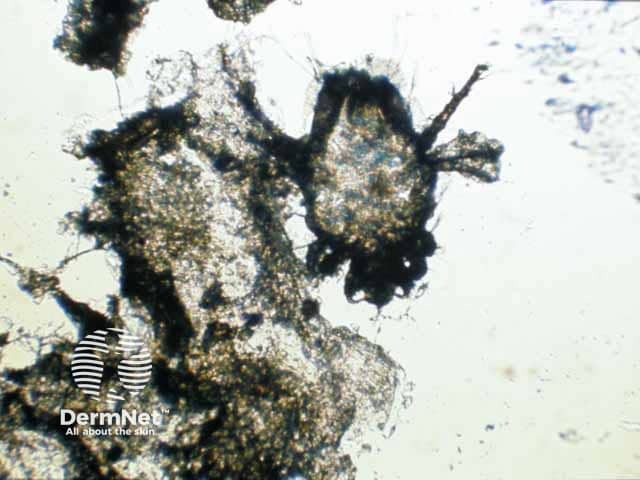
A scabies mite on microscopy after extraction from a burrow
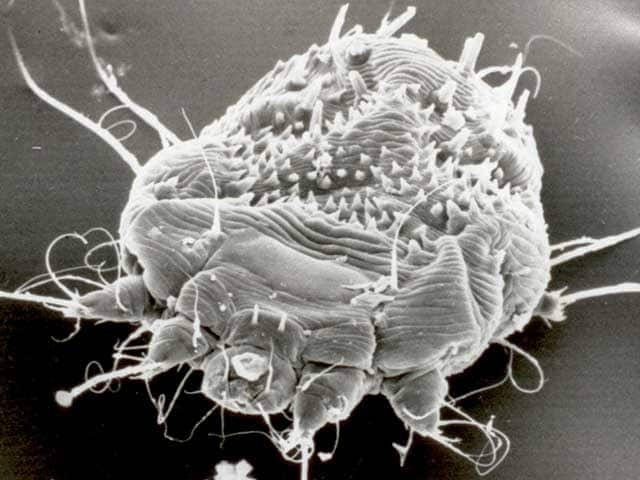
Scanning electron microscopy of Sarcoptes scabei
The International Alliance for the Control of Scabies (IACS) updated consensus criteria for the diagnosis of scabies in 2020, copied below:
It is important to note that all close contacts of a confirmed case of scabies should complete eradication therapy, whether they are symptomatic or not. Contacts may be infected but asymptomatic for several weeks, therefore they may continue to infect others and even reinfect the index case.
Classical scabies is associated with a good prognosis provided compliance is satisfactory and all close contacts (symptomatic or not) are simultaneously treated. Crusted scabies may need prolonged and repeated treatment and patients may have significant underlying conditions that will influence the prognosis. Pyococcal infection of scabies is one of the most common causes of acute glomerulonephritis globally.
Scabies reinfection is common and is usually secondary to spread from untreated close contacts. Repetitive use of disinfectants can lead to irritant dermatitis, and in the mistaken belief of continued scabies infestation, yet more disinfectant is used.