Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Last Reviewed: August, 2025
Author: Dr Lauren Thomas, Dermatology Registrar, Flinders Medical Centre, Australia (2025)
Previous authors: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, NZ (2016)
Peer reviewed by: Dr Tessa Li Chyin Lim, Australia (2025)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Treatment and prevention
Outcome
Crusted scabies (previously known as Norwegian scabies) is a highly contagious and severe form of scabies. It is caused by a hyperinfestation of Sarcoptes scabiei var. hominis, a type of scabies mite.
The term ‘crusted scabies’ may be considered a misnomer, as patients typically develop hyperkeratosis rather than true crusts (dried exudates).

Hyperkeratotic plaques on the thumb and palms

Hyperkeratotic plaques on the fingers with fissuring and nail dystrophy

Hyperkeratosis has extended over the trunk
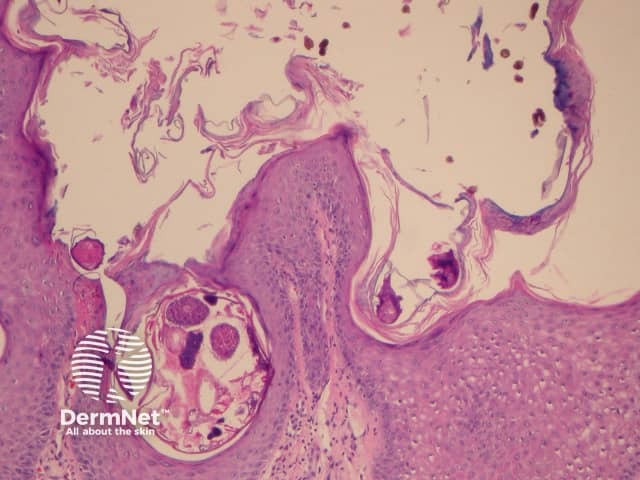
Scabies mites and eggs on palmar biopsy
Early crusted scabies on the palms in an elderly care home resident (SCAB-patient1)

Hyperkeratosis and fissuring on the feet in advanced crusted scabies
This severe form of scabies is more likely to occur in individuals with impaired immunological and mechanical defence mechanisms, resulting in uncontrolled mite proliferation.
Risk factors include:
Crusted scabies is caused by a hyperinfestation of Sarcoptes scabiei var. hominis. It is transmitted through direct contact with an infested individual or via contaminated fomites eg, bedding, clothing, furniture.
Host immune suppression allows the Sarcoptes mites to quickly spread and proliferate across the body. Individuals with crusted scabies can harbour up to 4,000 mites per gram of skin, totalling over 1 million mites. By comparison, individuals with typical scabies are only infected with 10–20 mites.
Crusted scabies may begin as poorly defined red or grey patches that develop into thick, scaly plaques. These plaques are typically found between the fingers, under the nails, or diffusely on the palms and soles. Common areas also include the elbows and knees.
Mites can accumulate in the nail beds, causing nail disorders such as nail thickening, discolouration, onycholysis, and dystrophy.
Pruritus may be minimal or absent due to the immunocompromised nature of the individual. Various factors can contribute to reduced scratching, including:
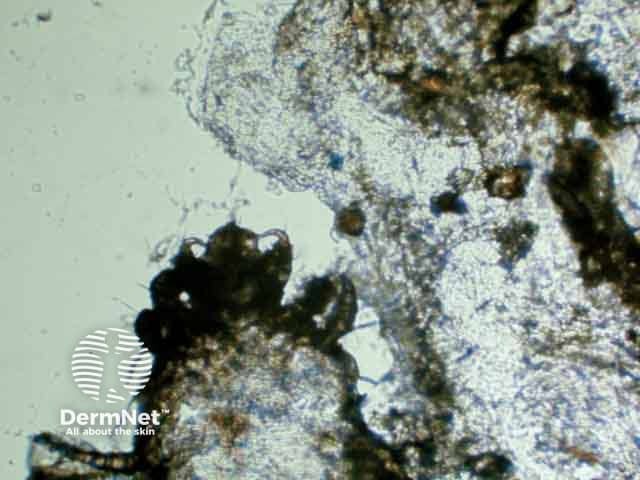
Diagnosis is confirmed by identifying mites or eggs through microscopic examination of skin scrapings. In addition, diagnosis is also supported by evidence of hyperkeratosis.
Reflectance confocal microscopy, where available, may assist in examining for burrows, mites, eggs, and mite faeces.
Skin biopsy is rarely needed, but histology typically shows multiple mites within the thickened stratum corneum. The dermis shows infiltration by lymphocytes and eosinophils, with a higher ratio of CD8+ lymphocytes than normal.
See also: scabies pathology.
Other investigations to consider in a patient with suspected crusted scabies:
Once crusted scabies is confirmed, consider further tests such as:
Management of the patient and their contacts should involve a dermatologist or infectious disease specialist. Treatment should occur in an inpatient or residential setting, with the patient in a private room. Nails, which can harbour mites, should be trimmed at the beginning of the hospital admission. Healthcare staff should adhere to contact precautions and wear full personal protective equipment, including shoe and hair covers.
Treatment of crusted scabies requires both oral ivermectin and topical preparations, alongside adjunctive measures.
The following grading system, devised at the Royal Darwin Hospital, may be used to determine the appropriate ivermectin treatment regimen:
Ivermectin is typically dosed at 200 μg/kg for adults and for children aged ≥5 years and weighing at least 15 kg, rounded to the nearest 3 mg tablet. It is taken after a fatty meal to aid absorption.
(Note: Ivermectin should not be given to pregnant or breastfeeding women, or children weighing less than 15 kg. Expert consultation is advised in such cases.)
In patients experiencing a second episode of crusted scabies within three months, a dose of 300 μg/kg may be considered, ideally in consultation with a specialist.
In addition to oral treatment, a topical scabicide is applied every second day for the first week, then twice a week until the condition resolves:
Topical scabicides should be applied to the entire body surface (excluding the eyes and mouth) and then left on for 24 hours. A toothbrush can be used to apply scabicide under the nails. Skin should be clean, dry, and cool before application.
Tea tree-based washes or antiseptic wash products may be considered, though evidence is limited and not routinely recommended in treatment guidelines.
Keratolytic creams are used in conjunction with topical scabicides to aid scabicide penetration. Keratolytics are applied to hyperkeratotic, scaly areas on alternate days:
Patients should be regularly re-examined to determine when to cease topical treatment, typically when hyperkeratotic areas have resolved. Repeat scrapings may be required if treatment response is inadequate.
All close contacts of a confirmed case of crusted scabies should simultaneously undergo eradication therapy, whether they are symptomatic or not. Infected contacts may remain asymptomatic for several weeks and therefore could continue to infect others and even reinfect the index case.
Close contacts can include family or household members, sexual partners, facility cohabitants or staff members, sports team members, or anyone who has shared items with someone infected.
Mites can survive for three days away from a human host; they can survive longer at lower temperatures and high humidity. Living areas should be thoroughly cleaned, as crusted plaques containing mites will commonly be shed. Linen, mattresses, and other bedding should also be cleaned regularly.
Pruritus can persist for several weeks following successful eradication. Itching can be managed with treatment such as antihistamines and topical steroids.
Crusted scabies can be effectively treated, but patients remain at risk of reinfestation, particularly if they are immunocompromised or their living conditions promote transmission. Ongoing education and regular follow-up are essential to monitor treatment success and prevent reinfestation.
The mortality rate is notably higher in older patients with crusted scabies compared to patients with typical scabies. Sepsis is the most common cause of scabies-related deaths.