Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Caroline Mahon, Dermatology and Paediatric Registrar, Auckland, New Zealand. 2013. Updated: Dr Ian Coulson, Consultant Dermatologist, Lancashire, UK. April 2022.
Introduction
Causes
Symptoms
Associated rashes
Diagnosis
Treatment
Treatment - skin manifestations of M. pneumoniae infection
Mycoplasma pneumoniae is a bacterial organism that unlike other bacteria lacks a cell wall. It causes respiratory tract infections.
Infection is spread by contact with droplets released from the upper and lower respiratory tracts of infected persons. The incubation period varies from 1–3 weeks. M. pneumoniae is a common cause of community-acquired pneumonia worldwide. Immunity after mycoplasma infection is short lived and it is possible to develop recurrent infections.
In many cases, infection due to M. pneumoniae is asymptomatic or results in non-specific symptoms such as headache, low-grade fever, dry cough and malaise. The respiratory examination is often normal, though scattered crepitations (crackles) and wheeze may be detected on listening to the chest with a stethoscope. However, it can lead to pneumonia, a serious lung infection.
M. pneumoniae can also result in complications in other organ systems, as a result of direct invasion by the bacteria or the immune response to the infection. The complications are sometimes more severe than the primary respiratory infection.
Some mycoplasma-associated illnesses are listed in the table below.
Organ system |
Symptoms and diseases caused by mycoplasma |
|
|---|---|---|
Respiratory system |
|
|
Nervous system |
|
|
Liver |
|
|
Heart |
|
|
Blood system |
|
|
Musculoskeletal system |
|
|
Gastrointestinal system |
|
|
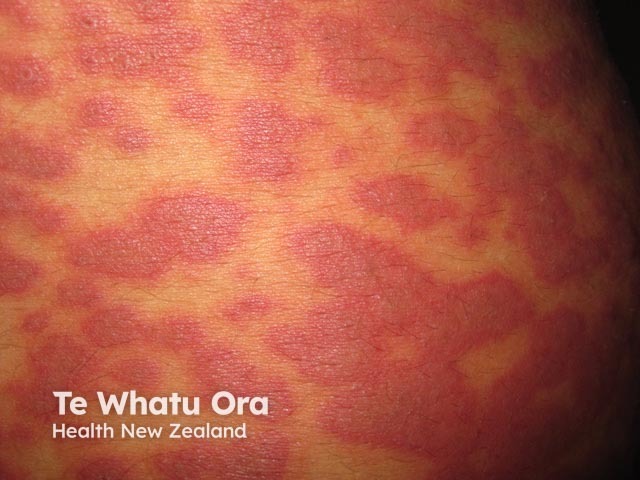
Rashes affect up to one-third of patients with M. pneumoniae respiratory tract infection.
The most frequent rash is non-specific exanthem in which short-lasting red patches appear on trunk and limbs. These areas of erythema clear by themselves and do not require specific treatment.
Vesicles and bullae, petechiae (small purple spots due to bleeding into the skin) and urticarial rashes (hive-like) have also been described in association with M. pneumoniae infection.

Bullae due to mycoplasma

Bullae due to mycoplasma
M. pneumoniae may occasionally cause bullous erythema multiforme (EM; EM major). Several specific features are typically present.

Atypical erythema multiforme due to mycoplasma
Atypical erythema multiforme due to mycoplasma

Target lesions associated with mycoplasma infection
Stevens–Johnson syndrome (SJS) / toxic epidermal necrolysis (TEN) are now considered manifestations of the same rare, acute, serious skin reaction in which there is sheet-like skin and mucosal loss. Conventional terminology describes SJS having skin detachment <10% of body surface area (BSA), TEN when it is >30% of BSA, and overlap when detachment is between 10% and 30%. Most cases are caused by medications.
M. pneumoniae is the most commonly-identified infectious cause of SJS, particularly in children and adolescents. In a recent retrospective review of all SJS cases seen at the Mayo clinic in the USA over a period of 8 years, 22% of cases were found to be associated with M. pneumoniae infection. The median age of this group was 14 years with a range of 10–36 years.
Rarely, M. pneumoniae has been associated with toxic epidermal necrolysis.
M. pneumoniae has rarely been associated with oral mucositis (stomatitis), conjunctivitis and genital mucous membrane ulceration, without an accompanying skin rash. This presentation has been variously named ‘atypical’ or ‘incomplete’ SJS (Fuchs syndrome), though it has been postulated that a more appropriate term for this syndrome is ‘mycoplasma-associated mucositis’. It usually affects children and young adults.

Mucositis due to mycoplasma
M. pneumoniae infection has been associated with a mucosal eruption often with minimal skin changes, that is distinct from Stevens-Johnson syndrome and erythema multiforme. In a review of 202 cases, affected patients were young with an average of 12 years of age, and skin lesions were either absent (34%) or sparse (47%). Oral, ocular and urogenital lesions (94%, 82% and 63% respectively) predominated. Skin lesions were either vesiculobullous or target-like, and usually situated acrally.
The reaction can be classified as:
The authors stressed that a key distinction from herpesvirus or drug-induced Stevens-Johnson or toxic epidermal necrolysis was the relative sparsity of skin lesions.
Although the mucosal lesions may scar, the overall prognosis was good.
MIRM has since been subsumed under the umbrella term 'reactive infectious mucocutaneous eruption (RIME)'.
M. pneumoniae infection has also been reported in association with several other skin problems, including:
Clinical suspicion of M. pneumoniae infection arises in a patient with a respiratory illness and any type of rash, but especially an erythema multiforme-like eruption.
The most rapid diagnostic test is M. pneumoniae polymerase chain reaction (PCR) of a throat swab, which has a sensitivity and specificity of 78–100%.
Mycoplasma serology (a blood test) detects IgM and IgG antibodies after a 7–10 days and 3 weeks respectively. The sensitivity and specificity of serologic testing is lower than PCR (50–66%) but can be increased by arranging a second test in the convalescent phase of the illness. A positive test is confirmed if a single titre is >1:32 or a fourfold increase in an IgG or IgM titre from baseline is found on repeat testing. IgM titres remain raised for weeks, and IgG remains raised for many months after mycoplasma infection.
Chest x-ray findings in M. pneumoniae infection are non-specific. Most commonly, there is patchy consolidation in one or both lungs. Small pleural effusions (fluid in the lining of the lungs) may be seen in up to 20% of cases.
The results of routine blood testing are also non-specific. The total white cell count, and differential counts may be within normal limits. Inflammatory marker testing may reveal normal, or elevated CRP and ESR levels. There may be mild, non-specific abnormalities in the liver function test results.
Full blood count testing may reveal:
Mycoplasma infection is usually treated with a macrolide antibiotic, usually erythromycin or roxithromycin. These reduce infectivity to others, and may improve respiratory symptoms as well as associated skin rash.
Clarithromycin, and azithromycin are more expensive, and may require approval from an infectious diseases physician for their use in New Zealand. They require less frequent dosing than erythromycin or roxithromycin, and are less likely to result in gastrointestinal side effects.
Alternatives in patients allergic to, or unable to tolerate macrolides, or for which there is a potential medication interaction, are doxycyline or moxifloxacin.
No vaccine is available for M. pneumoniae infection.
Non-specific rashes due to mycoplasma infection can be treated with bland emollients to reduce discomfort.
Oral antihistamines may be helpful for urticaria.
Expert advice should be sought if there are blisters or mucous membrane involvement. In patients with erythema multiforme, supportive care and close observation is essential.