Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Vanessa Ngan, Staff Writer, 2003.
Introduction - naevus Introduction - Ota, Ito and Hori naevi Causes and demographics Signs, symptoms and complications Diagnosis Treatment
A naevus (American spelling nevus, nevi) is a circumscribed and stable malformation of a component of the skin. Naevi (American spelling nevi) are often present at birth, when they are often called brown birthmarks. Naevi composed of melanocytes (the pigment cells that produce melanin) are called melanocytic naevi or pigmented naevi.
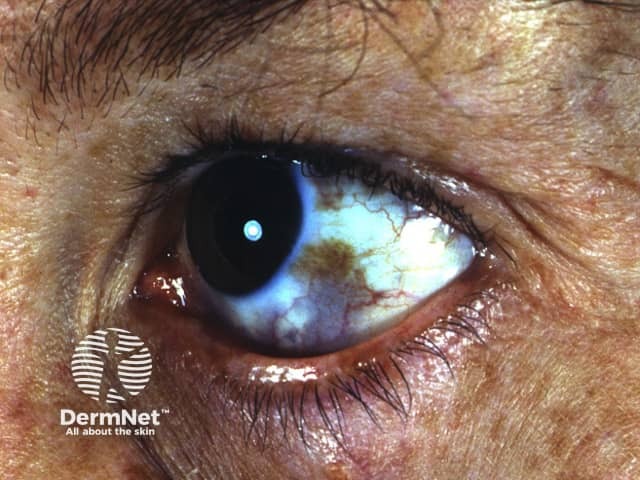
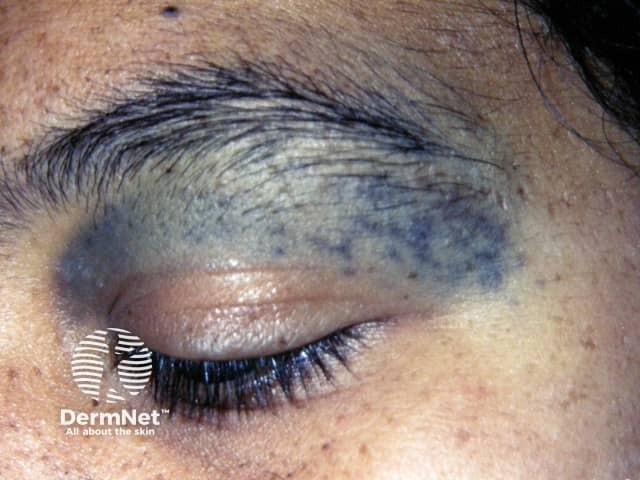
Naevus of Ota, naevus of Ito and naevus of Hori are special melanocytic naevi that have a slate-brown or blue/grey colouring. They are forms of dermal melanocytosis in which naevus cells are found deep within the dermis.
Dermal melanocytosis can also occur elsewhere on the body, including inside the mouth.
Naevus of Ota
Naevus of Ota

Naevus of Ota

Naevus of Ito

Naevus of Ito
It is not known why dermal melanocytosis occurs. Specific mutations have been detected within the dermal melanocytes, most often GNAQ or GNA11. Researchers have suggested that hormones play a part in their development. The role of ultraviolet radiation is thought to be small, as it does not reach deep dermal melanocytes.
Naevus of Ota is much more common than naevus of Ito. These naevi are present at birth in 50% of cases but may appear during adolescence or adult life. Naevus of Hori is not present at birth and is therefore a form of acquired melanocytosis.
Naevi of Ota and Ito are most commonly found in Asian populations; 0.2–0.6% of Japanese people have a naevus of Ota. They appear more frequently in females. Both forms of naevi are uncommon in Caucasians.
In all forms of dermal melanocytosis:
The diagnosis of dermal melanocytosis is usually made by observing typical discolouration of the skin. It is classified according to the site affected.
Some patients may undergo skin biopsy, which confirms the presence of melanocytes in the dermis.
Other skin conditions resulting in bluish or grey coloured skin may be considered. These include:
Treatment of a melanocytosis may include cosmetic camouflage to cover the disfiguring markings, and laser treatment (usually using 1064nm Q switched Nd:YAG, Alexandrite or QS ruby laser) or intense pulsed light (IPL).
If the eye is affected, regular eye examinations should be arranged to detect glaucoma. Any change in a naevus should be assessed by a dermatologist.