Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Last Reviewed: February, 2025
Author: Dr Selene Ting, Dermatology Advanced Trainee, Monash Medical Centre, Australia (2025).
Previous contributors: Hon A/Prof Amanda Oakley, Dermatologist, New Zealand (1997); Dr Anita Eshraghi, Dermatologist, Sweden, (2018)
Peer reviewed and updated by: Dr James A. Ida, MD, MS, Dermatologist, USA (2025)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Eruptive naevi
Treatment
Outcome
A blue naevus (nevus in American spelling) is a type of melanocytic naevus in which spindle-shaped or, less commonly, ovoid naevus cells are located most often wholly but at least partially within the dermis.
Different subtypes of blue naevi include:

A blue naevus - the monochrome slate blue colour is typical

Blue naevi on the arm and nose

A blue naevus on the hand (BlueN-patient16)
Click here for more images of blue naevi
Blue naevi are twice as common in women compared to men. They are more common among Asians, with a prevalence between 3–5% compared to approximately 1–2% among Caucasian adults. They are rarely found at birth or within the first two years of life.
Congenital blue naevi are present in about 1 in 3000 neonates. Most become evident later in childhood or adolescence.
Blue naevi derive from the incomplete migration of melanocytes from the neural crest to the skin during foetal development. The melanocytes of blue naevi are located deeper in the skin within the dermis as compared to those of brown naevi, which are located in the more superficial epidermis.
It has been held that the deeper location of dermal melanocytes in blue naevi causes their colour to be perceived by the eye as bluish. This phenomenon has classically been extrapolated to be due to the Tyndall effect, which posits that shorter (blue) wavelengths of incident light are preferentially scattered by the deeper-located dermal melanocytes; this is in contrast to the more superficially located epidermal melanocytes which appear brown.
A more recent study, however, has suggested that the perception of blue colour in blue naevi may be more aptly regarded as a relative decrease in scatter of higher wavelength red light rather than as an increase in scatter of lower wavelength blue light. Thus, these authors conclude that blue naevi are perceived as blue because they scatter less red light, leading to a shift in hue toward blue (“subtractive colour mixing”), rather than because they scatter more blue light.
Common blue naevi do not have any complications. They are benign and remain unchanged throughout life.
In contrast, cellular blue naevi can rarely transform into malignant cellular blue naevi (a type of melanoma).
Blue naevi are usually diagnosed clinically by their typical appearance. The diagnosis may be confirmed by finding a homogeneous, steel-blue, hazy or ground-glass pattern on dermoscopy.

Dermoscopy of a blue naevus (BlueN-patient3)

Dermoscopy of a blue naevus (BlueN-patient7)
Click here for more images of blue naevi
If there is any uncertainty about the diagnosis, an excisional biopsy may be performed. The histopathology of blue naevus reveals spindle-shaped melanocytes in the mid-dermis, made of epithelioid cells with heavily pigmented cytoplasm. SOX10 and Melan-A stains are positive.
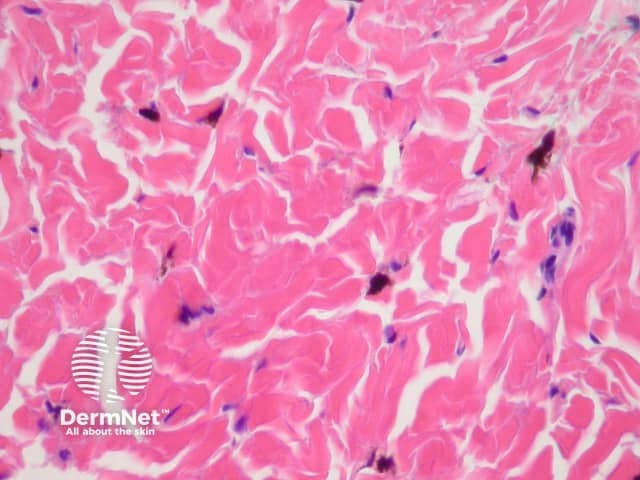
Histopathology of dermal dendritic melanocytes that make up a common blue naevus
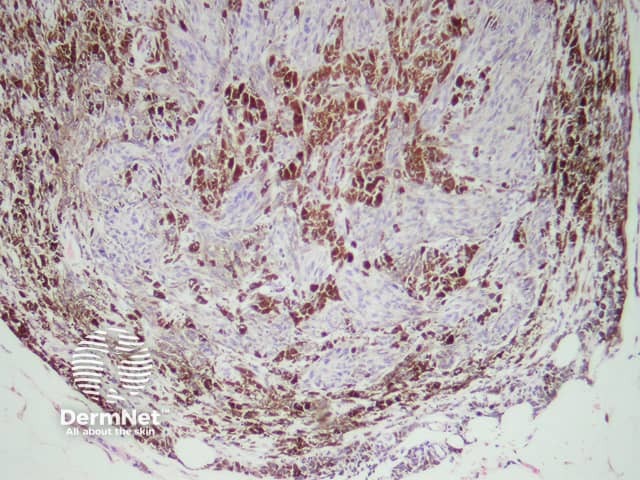
Histopathology of a cellular blue naevus - cells may be round oval or fusiform

Blue naevus

Blue naevus
The differential diagnosis of blue naevi includes:
Eruptive blue naevi present as a sudden, rapid appearance of clustered, blue-grey naevi at various anatomical sites in immunosuppressed patients or in those with a blistering disorder or cutaneous injury. They have been reported at sites of herpes zoster and have been associated with puberty, pregnancy, and severe sunburns.
Eruptive blue naevi can occur in individuals of any Fitzpatrick skin type, with no reported racial predilection.
Usually, no treatment is required.
Blue naevi that are larger than 1 cm, change or appear de novo in an adult should be considered for histological evaluation to exclude melanoma. Blue naevi of the scalp are often removed as a precaution because their history is frequently unknown and they are difficult to monitor. They may also be surgically removed for cosmetic reasons.
Unless surgically removed, blue naevi typically persist lifelong.