Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Bromhidrosis — extra information
Bromhidrosis
Authors: Vanessa Ngan, Staff Writer, 2005; Updated: Dr Maanasa Bandla, Hospital Intern, Monash Health, Melbourne, Australia; Dr Martin Keefe, Dermatologist, Christchurch, New Zealand. Copy edited by Gus Mitchell. June 2021
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is bromhidrosis?
Bromhidrosis, also known as osmidrosis or ozochrotia, is an unpleasant or offensive body odour due to any cause including poor hygiene, infections, diet or medications, or inherited metabolic disorders. It may be associated with hyperhidrosis.
Who gets bromhidrosis?
Bromhidrosis can affect all age groups, races, and both sexes. Bromhidrosis is more common in adults than children as sebaceous glands and apocrine sweat glands do not become active until puberty. The elderly have a different body odour from babies, pre-pubescent children, teenagers, and adults. It has a male predominance, and can be a particular issue in hot humid tropical climates. There may be a genetic predisposition, with studies suggesting axillary malodour is more common in Europeans and Africans than Asians.
What causes bromhidrosis?
Body odour is normal and is primarily produced by the breakdown of sweat, sebum, and keratin by bacteria on the skin surface (skin microbiota). What is regarded as acceptable is determined by cultural influences including race and social upbringing.
Bromhidrosis may be classified as eccrine or apocrine, exogenous or endogenous:
- Eccrine bromhidrosis
- Eccrine glands are distributed over most of the skin surface.
- Eccrine sweat is secreted continuously and is normally odourless.
- Eccrine sweat is important in thermoregulation.
- Apocrine bromhidrosis
- Apocrine glands are located in the axillae, anogenital region, and breasts, and become active in puberty.
- Apocrine sweat is secreted intermittently and is normally odourless.
- Apocrine sweat is controlled by the sympathetic nervous system.
- Exogenous
- Skin microbiota — Corynebacterium species, Staphylococcus hominis, S epidermidis, Cutibacterium avidum, Acinetobacter schindleri.
- Skin infections — erythrasma, pitted keratolysis, trichomycosis, Sphingomonas paucimobilis.
- Nasal foreign body.
- Endogenous
- Foods — garlic, onion, asparagus, curry, alcohol.
- Medications and toxins — penicillin, bromides, dupilumab.
- Systemic and skin disorders — obesity, diabetes mellitus, liver disease, renal failure, skin disorders of palms/soles and flexures.
- Metabolic disorders — trimethylaminuria, phenylketonuria, hypermethioninaemia.
What are the clinical features of bromhidrosis?
Bromhidrosis presents as a bad body smell which the patient may be unaware of. Malodour may be the reason for the consultation, raised by a mother or partner, or be obvious during a medical consultation for other reasons. The odour may be worse after exercise, often adhering to clothing.
Apocrine bromhidrosis is the most common form of bromhidrosis in adults and is localised, usually to the armpits and/or anogenital area.
Eccrine bromhidrosis presents as a generalised malodour, and may be associated with bad breath (halitosis), anogenital odour, and smelly urine.
Specific sites and features to look for on examination:
- Hyperhidrosis
- Skin folds — intertrigo, erythrasma, flexural dermatoses
- Body hair (particularly axillary) — trichomycosis
- Hands and feet — pitted keratolysis, palmoplantar keratoderma
- Inside the nose for foreign body.

Underarm sweating

Trichomycosis axillaris
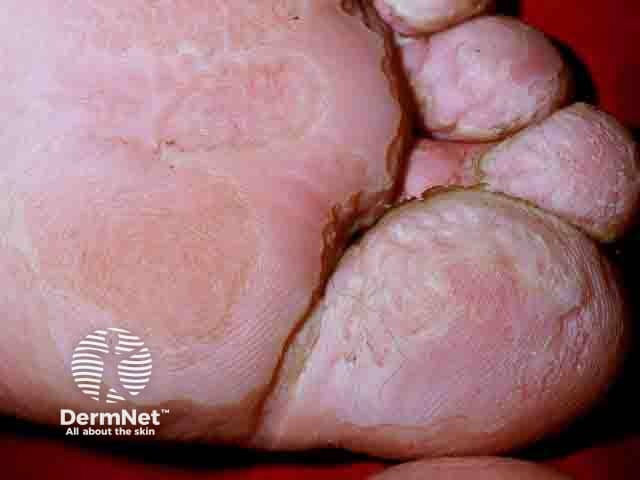
Macerated skin over the toes and ball of the foot in pitted keratolysis
What are the complications of bromhidrosis?
Bromhidrosis can have a significant impact on quality of life, causing:
- Anxiety
- Low self-esteem
- Social withdrawal.
How is bromhidrosis diagnosed?
Bromhidrosis is a clinical diagnosis, but careful history and examination is required to determine the underlying cause. Investigations should be considered in children, if the smell is generalised also involving urine and breath, or if it is of recent onset unrelated to hygiene habits.
The clinician who notices a strong body odour is wise to tread carefully when broaching the subject but correct diagnosis and treatment has the potential to be life-changing for the patient.
What is the differential diagnosis for bromhidrosis?
- Body dysmorphophobia
- Olfactory hallucinations (due to neurological or psychiatric disorders)
- Olfactory refractory syndrome (fear of having an offensive body odour)
What is the treatment for bromhidrosis?
General measures
- Good hygiene with regular washing using soaps and cleansers, deodorant, antiperspirant, removal of sweaty clothing
- Hair removal by shaving, electrolysis, or lasers
- Topical antiseptics
- Exfoliation of areas of keratin degradation
Specific measures
- Avoidance of odour-causing foods and medications
- Treatment of skin infections
- Treatment of hyperhidrosis
- Removal of nasal foreign body
- Removal of apocrine glands — laser, surgery, liposuction curettage, microwave-induced fibrosis
- Dietary modification for metabolic disorders
What is the outcome for bromhidrosis?
Fixing bromhidrosis due to poor hygiene or other treatable causes can be life-changing. However not all cases of malodorous body odour can be completely suppressed.
Bibliography
- Lam TH, Verzotto D, Brahma P, et al. Understanding the microbial basis of body odor in pre-pubescent children and teenagers. Microbiome. 2018;6(1):213. doi:10.1186/s40168-018-0588-z. Journal
- Lanzalaco A, Vanoosthuyze K, Stark C, Swaile D, Rocchetta H, Spruell R. A comparative clinical study of different hair removal procedures and their impact on axillary odor reduction in men. J Cosmet Dermatol. 2016;15(1):58–65. doi:10.1111/jocd.12197. Journal
- Lucky AW. Acquired bromhidrosis in an 8-year-old boy secondary to a nasal foreign body. Arch Dermatol. 1991;127(1):129. doi:10.1001/archderm.1991.01680010141033. PubMed
- Malik AS, Porter CL, Feldman SR. Bromhidrosis treatment modalities: a literature review. J Am Acad Dermatol. 2021;S0190-9622(21)00175-4. doi:10.1016/j.jaad.2021.01.030. PubMed
- Mogilnicka I, Bogucki P, Ufnal M. Microbiota and malodor - etiology and management. Int J Mol Sci. 2020;21(8):2886. doi:10.3390/ijms21082886. Journal
- Patel F, Tu YM, Fernandes S, Chapas A. A case of axillary bromhidrosis secondary to trimethylaminuria successfully treated with microwave-based therapy. JAAD Case Rep. 2019;5(10):915–17. doi:10.1016/j.jdcr.2019.07.018. PubMed Central
- Rowane M, Valencia R, Schend J, Jhaveri D, Hostoffer R. Something to sweat about: two cases of dupilumab-induced hyperhidrosis and bromhidrosis. Allergy Rhinol (Providence). 2020;11:2152656720927703. doi:10.1177/2152656720927703. PubMed Central
- Salim G, Zahra MF. Trichobacteriosis: contribution of dermoscopy. Dermatol Online J. 2014;20(9):13030/qt7488g7vb. PubMed
- Scarff CE. Sweaty, smelly hands and feet. Aust Fam Physician. 2009;38(9):666–9. PubMed
- Semkova K, Gergovska M, Kazandjieva J, Tsankov N. Hyperhidrosis, bromhidrosis, and chromhidrosis: fold (intertriginous) dermatoses. Clin Dermatol. 2015;33(4):483–91. doi:10.1016/j.clindermatol.2015.04.013. PubMed
On DermNet
Other websites
- Bromhidrosis — Medscape Reference
