Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Dr Amritpreet Singh, Advanced Trainee in General Medicine, Wellington Regional Hospital, New Zealand; A/Prof Amanda Oakley, Dermatologist, Waikato District Health Board, Hamilton, New Zealand. Copy edited by Gus Mitchell. March 2022
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
Fournier gangrene is a polymicrobial, rapidly progressive necrotising fasciitis of the external genitalia, perineum, and perianal region.
It is also known as Fournier disease and necrotising fasciitis of the perineum and genitalia.
Fournier gangrene may be subcategorised by the site of infection:
Fournier gangrene is a surgical emergency associated with septic shock, which requires prompt surgical excision and broad-spectrum intravenous antibiotics.
Fournier gangrene is rare, with an incidence of 1.6 in 100,000 males. The male to female ratio is 10:1. The lower incidence in females may reflect better drainage of the perineal region.
The typical patient with Fournier gangrene is a male aged 50–79 with comorbid conditions that compromise cellular immunity. These comorbid conditions include:
The risk of contracting Fournier gangrene may be increased by the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors such as empagliflozin for the treatment of type 2 diabetes. These inhibitors can promote the growth of baseline urogenital flora and the risk of localised infection.
Fournier gangrene originates from a local urogenital or anorectal infection, such as:
Bacteria gain entry into the superficial and deep perineal fascia through trauma, such as:
Infection or trauma is identifiable in 95% of cases of Fournier gangrene.
Once the infection is introduced to the fascia, bacterial toxins are released. These promote thrombosis of arterioles, causing necrosis of the fascia and localised ischaemia. The resultant tissue hypoxia promotes the growth of anaerobic organisms, which produce gas and enzymes leading to further necrosis of the fascia.
Fournier gangrene is polymicrobial in 80% of cases, with an average of four microorganisms per infection, including:
Fever and lethargy may be present for 2–7 days before visible changes in the skin. Fournier gangrene has the following clinical features:
The initial appearance of the skin may underestimate the severity of the disease.
The testicles, penis, and urethra are not commonly involved due to their autonomous blood supply.
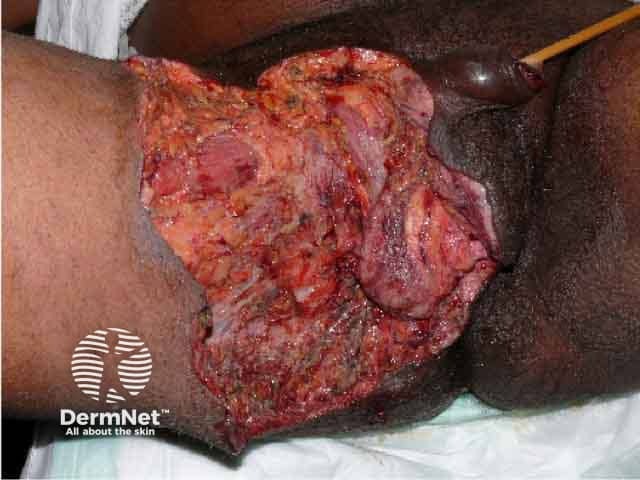
Fournier gangrene after debridement of necrotic tissue

Fournier gangrene after debridement of necrotic tissue

Fournier gangrene after healing both by secondary intention and skin grafts

Fournier gangrene showing dusky oedema of the scrotum and penis and epidermal necrosis over the groin
The complications of Fournier gangrene include:
Fournier gangrene should be suspected if fluctuance, soft tissue crepitation, localised tenderness of wound are detected on examination of the genitalia and perineum. It is confirmed if gangrenous tissue or pus is found. Examination under anaesthesia may be needed.
Thrombosis of arterioles supplying the superficial and deep fascia is histologically pathognomonic of Fournier gangrene.
Computed tomography (CT scan) defines the extent of disease and reveals fascial thickening, fat stranding, and soft tissue gas collections.
The differential diagnosis of Fournier gangrene includes:
Fournier gangrene is a surgical emergency. Immediate surgical intervention is imperative if gas is detected clinically or on a CT scan.
Once the infection has been eradicated and healthy granulation tissue has developed, the defect should be reconstructed by primary closure, local skin flap, or a split-thickness skin graft.
A combination of broad-spectrum intravenous antibiotics is required. For example:
Fournier gangrene is life-threatening and fatal without appropriate treatment.
Diagnosis is often delayed due to the insidious onset of symptoms. The mortality rate is 20–40%. The most common cause of death is septic shock.
Patients often require repeated surgical excisions and remain hospitalised for weeks to months. The minimum time from surgical excision to reconstruction is approximately three weeks.
Following reconstruction, the prognosis of Fournier gangrene is good. However, 50% of men with penile involvement report ongoing pain with erections. If extensive soft tissue is lost, lymphatic drainage may be impaired, resulting in oedema and recurrent cellulitis.