Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Fournier gangrene — extra information
Fournier gangrene
Authors: Dr Amritpreet Singh, Advanced Trainee in General Medicine, Wellington Regional Hospital, New Zealand; A/Prof Amanda Oakley, Dermatologist, Waikato District Health Board, Hamilton, New Zealand. Copy edited by Gus Mitchell. March 2022
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is Fournier gangrene?
Fournier gangrene is a polymicrobial, rapidly progressive necrotising fasciitis of the external genitalia, perineum, and perianal region.
It is also known as Fournier disease and necrotising fasciitis of the perineum and genitalia.
Fournier gangrene may be subcategorised by the site of infection:
- Fournier gangrene of the penis
- Fournier gangrene of the scrotum or perineum
- Fournier gangrene of the vagina
- Fournier gangrene of the vulva or perineum.
Fournier gangrene is a surgical emergency associated with septic shock, which requires prompt surgical excision and broad-spectrum intravenous antibiotics.
Who gets Fournier gangrene?
Fournier gangrene is rare, with an incidence of 1.6 in 100,000 males. The male to female ratio is 10:1. The lower incidence in females may reflect better drainage of the perineal region.
The typical patient with Fournier gangrene is a male aged 50–79 with comorbid conditions that compromise cellular immunity. These comorbid conditions include:
- Diabetes mellitus (present in 60% of cases)
- Alcoholism
- Cirrhosis of the liver
- Systemic lupus erythematosus
- Crohn disease
- Human immunodeficiency virus (HIV) infection
- Morbid obesity.
The risk of contracting Fournier gangrene may be increased by the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors such as empagliflozin for the treatment of type 2 diabetes. These inhibitors can promote the growth of baseline urogenital flora and the risk of localised infection.
What causes Fournier gangrene?
Fournier gangrene originates from a local urogenital or anorectal infection, such as:
- Urinary tract infection, epididymitis, or orchitis
- Perianal, perirectal, or ischiorectal abscess
- Vaginal, vulval, or Bartholin gland abscess.
Bacteria gain entry into the superficial and deep perineal fascia through trauma, such as:
- A genital piercing
- Urethral instrumentation or injury
- A prosthetic penile implant
- A rectal foreign body
- Post-coital trauma
- Colorectal trauma during surgery.
Infection or trauma is identifiable in 95% of cases of Fournier gangrene.
Once the infection is introduced to the fascia, bacterial toxins are released. These promote thrombosis of arterioles, causing necrosis of the fascia and localised ischaemia. The resultant tissue hypoxia promotes the growth of anaerobic organisms, which produce gas and enzymes leading to further necrosis of the fascia.
Fournier gangrene is polymicrobial in 80% of cases, with an average of four microorganisms per infection, including:
- Escherichia coli (most common aerobe)
- Bacteroides (most common anaerobe)
- Proteus
- Staphylococcus
- Streptococcus
- Pseudomonas.
What are the clinical features of Fournier gangrene?
Fever and lethargy may be present for 2–7 days before visible changes in the skin. Fournier gangrene has the following clinical features:
- Tachycardia and hypotension
- Severe genital pain
- Cyanosis, erythema, blistering, oedema, induration, and pruritus of the overlying skin
- Subcutaneous crepitus
- Wet gangrene with a feculent odour due to anaerobic infection.
The initial appearance of the skin may underestimate the severity of the disease.
The testicles, penis, and urethra are not commonly involved due to their autonomous blood supply.
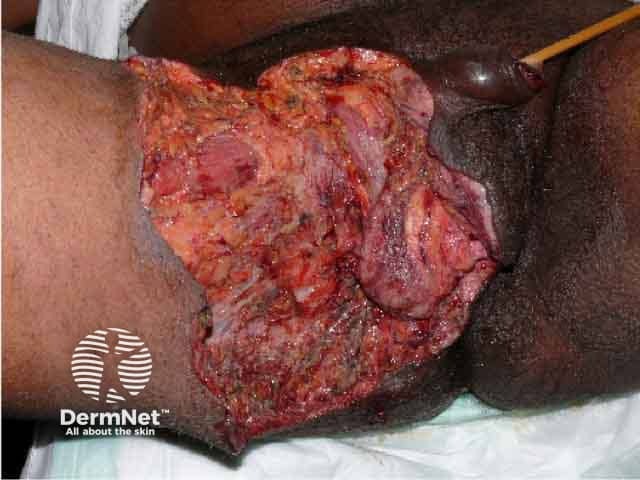
Fournier gangrene after debridement of necrotic tissue

Fournier gangrene after debridement of necrotic tissue

Fournier gangrene after healing both by secondary intention and skin grafts

Fournier gangrene showing dusky oedema of the scrotum and penis and epidermal necrosis over the groin
What are the complications of Fournier gangrene?
The complications of Fournier gangrene include:
- Septic shock
- Diabetic ketoacidosis
- Disseminated intravascular coagulation
- Acute kidney injury
- Multiple organ failure
- Prolonged hospital admission.
How is Fournier gangrene diagnosed?
Fournier gangrene should be suspected if fluctuance, soft tissue crepitation, localised tenderness of wound are detected on examination of the genitalia and perineum. It is confirmed if gangrenous tissue or pus is found. Examination under anaesthesia may be needed.
Thrombosis of arterioles supplying the superficial and deep fascia is histologically pathognomonic of Fournier gangrene.
Computed tomography (CT scan) defines the extent of disease and reveals fascial thickening, fat stranding, and soft tissue gas collections.
What is the differential diagnosis for Fournier gangrene?
The differential diagnosis of Fournier gangrene includes:
- Acute epididymitis
- Gangrenous balanitis
- Gangrenous vulvitis
- Cellulitis
- Orchitis
- Inguinal lymphogranulomatosis
- Soft chancre.
What is the treatment for Fournier gangrene?
Fournier gangrene is a surgical emergency. Immediate surgical intervention is imperative if gas is detected clinically or on a CT scan.
Surgical debridement and excision
- All necrotic tissue must be removed promptly.
- Repeated procedures may be necessary.
Once the infection has been eradicated and healthy granulation tissue has developed, the defect should be reconstructed by primary closure, local skin flap, or a split-thickness skin graft.
Antibiotics
A combination of broad-spectrum intravenous antibiotics is required. For example:
- Tazocin and clindamycin
- Tazocin and metronidazole
- Vancomycin instead of tazocin if methicillin-resistant Staphylococcus aureus (MRSA) is detected
- Meropenem instead of tazocin if the patient is allergic to penicillin.
Other specific measures
- Intravenous fluids
- Tetanus prophylaxis
- Consider intravenous immunoglobulin (IVIG)
- Consider hyperbaric oxygen therapy for clostridial involvement, myonecrosis, or failure of conventional treatment.
General measures
- Avoid nonsteroidal anti-inflammatory drugs.
- Address underlying comorbidities.
- Encourage perineal hygiene.
- Avoid urethral and rectal trauma or foreign body.
What is the outcome for Fournier gangrene?
Fournier gangrene is life-threatening and fatal without appropriate treatment.
Diagnosis is often delayed due to the insidious onset of symptoms. The mortality rate is 20–40%. The most common cause of death is septic shock.
Patients often require repeated surgical excisions and remain hospitalised for weeks to months. The minimum time from surgical excision to reconstruction is approximately three weeks.
Following reconstruction, the prognosis of Fournier gangrene is good. However, 50% of men with penile involvement report ongoing pain with erections. If extensive soft tissue is lost, lymphatic drainage may be impaired, resulting in oedema and recurrent cellulitis.
Bibliography
- Auerbach J, Bornstein K, Ramzy M, Cabrera J, Montrief T, Long B. Fournier Gangrene in the Emergency Department: Diagnostic Dilemmas, Treatments and Current Perspectives. Open Access Emerg Med. 2020; 12:353–364. DOI: 10.2147/OAEM.S238699. Journal
- Bersoff-Matcha S, Chamberlain C, Cao C, Kortpeter C, Chong W. Fournier Gangrene Associated with SGLT Inhibitors: A Review of Spontaneous Postmarketing Cases. Ann. Intern. Med. 2019; 170(11):764–769. DOI: 10.7326/M19–0085. Journal
- El-Qushayri AE, Khalaf KM, Dahy A, et al. Fournier’s gangrene mortality: a 17-year systematic review and meta-analysis. Int. J. Infect. Dis. 2020; 92:218–225. DOI: 10.1016/j.ijid.2019.12.030. Journal
- Kumar S, Costello AJ, Colman PG. Fournier's gangrene in a man on empagliflozin for treatment of Type 2 diabetes. Diabet Med. 2017; 34(11):1646–1648. DOI: 10.1111/dme.13508. Journal
- Pernetti R, Palmieri F, Sagrini E, et al. Fournier's gangrene: Clinical case and review of the literature. Arch Ital Urol Androl. 2016;88(3):237–8. Published 2016 Oct 5. doi:10.4081/aiua.2016.3.237. Journal
- Vaz I. Fournier gangrene. Trop Doct. 2006; 36(4):203–4. DOI: 10.1258/004947506778604724. Journal
On DermNet
- Fournier gangrene images
- Bacterial skin infections
- Fever and a rash
- Genital skin problems
- Hyperbaric oxygen therapy
- Necrotising fasciitis
- Necrotising fasciitis pathology
- Wet gangrene
Other websites
- Fournier gangrene — NORD Rare Disease Database.
- Safety announcement: FDA warns about rare occurrences of serious infection of the genital areas with SGLT2 inhibitors for diabetes — U.S Food and Drug Administration.
