Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Brian Wu PhD. MD Candidate, Keck School of Medicine, Los Angeles, USA; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, January 2016.
Introduction
Occupational risks
Causes
Irritant contact dermatitis
Latex allergy
Allergic contact dermatitis
Mechanical injury
Workplace risk assessment
Personal protective equipment
Hand care advice
Diagnosis and treatment
Dentists and dental technicians are considered to be in a high-risk profession for occupational dermatoses. In one study out of Norway, for example, it was found that 40% of dentists suffer from job-related skin disorders, while a Belgian study found that 23% suffer from allergic contact dermatitis and 9% from chronic skin infections. An Australian study found that between 9% and 22% of those employed in dentistry suffer specifically from latex allergy.
Dentists and dental technicians are uniquely vulnerable to job-related skin problems.
According to the United States Bureau of Labor Statistics, skin diseases are the most common form of occupation-related illness and represent around 16.5% of all work-related illnesses and injuries. These problems occur when various occupational hazards compromise the protective barrier of the skin and lead to irritation/inflammation, itch and pain.
Dentists and dental technicians are particularly prone to latex allergy and contact dermatitis.
Irritant contact dermatitis is often associated with “wet work”, or the constant or frequent submerging of hands in water. It can lead to acute dermatitis, ie redness, weeping or swelling, and on to chronic dermatitis, ie dry, cracked or scaling skin.
Latex allergy is a Type 1 hypersensitivity reaction to latex proteins (contact urticaria) and in extreme cases can rarely be fatal. Diagnosis based on medical history which is typically immediate redness and swelling on exposure to latex gloves. Latex reactions can be severe, but generally resolve within an hour or so.
Allergic contact dermatitis can arise from dental materials, solids, lubricating oils and X-ray chemicals. Specific allergens include:

Hand dermatitis due to rubber glove allergy

Positive patch tests to acrylates in a dentist

Positive patch test to acrylate
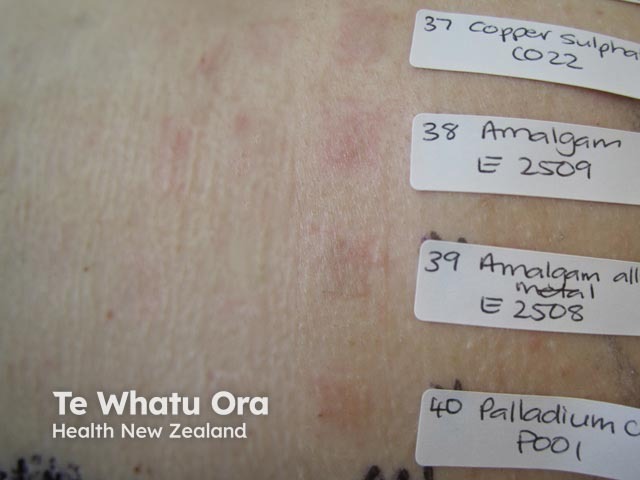
Borderline multiple patch tests in a dentist
Needle sticks and cuts/abrasians from sharps account for 50% of mechanical injuries in dentists and dental technicians. These are due to the small operating field, patient movement and the variety of sharps used. These injuries risk transmitting infection, including human immunodeficiency virus (HIV), hepatitis B and various bacteria.
Dental clinics and practices are highly regulated entities and this includes regulations for workplace risk. Agencies like the National Institute for Occupational Safety and Health (NIOSH) and similar regulatory bodies in other countries mandate employee education on infection control and prevention, sharps storage, use and disposal, safe handling of chemicals and cleaners used in dentistry and other aspects of workplace health.
Personal protective equipment (PPE) includes the use of face masks and gloves in the dental profession, mostly due to risk for transmission of viral illness, and to protect workers from exposure to potential irritants or allergens. However, many workers develop a sensitivity to latex or to other compounds in rubber gloves, and skin reactions related to prolonged wearing of face masks.
Increased use of non-latex gloves has led to a reduction in incidence of rubber allergy in dentists and dental technicians.
Hand care advice for dentists and dental technicians includes:
Diagnosis of occupational skin disorders should be based on:
Treatment of occupational skin disorders can include: