Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Scabies — extra information
Scabies
Author: Dr Jessica Rachel Maguire, IMT, Barts Health NHS Trust, London, United Kingdom, March 2022; updated by Dr Ian Coulson, Dermatologist, United Kingdom, April 2025.
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
What is scabies?
Scabies is a transmissible skin disease caused by the ectoparasitic mite Sarcoptes scabiei var. hominis. This variant infests humans only; scabies cannot be caught or transferred to other animals.
Scabies is a highly contagious infestation of the human epidermis. Scabies was described by Aristotle who likened the disease to ‘lice of the flesh’. Scabies presents as a rash with intense itching; it may have a characteristic appearance and distribution.
Who gets scabies?
Scabies is a global disease, and anyone can be affected. It is estimated that about 204 million people are affected by scabies worldwide, with an annual incidence of 455 million cases. Scabies is more common in the elderly, children, and adolescents.
The burden of disease is higher in low-income areas, in the tropics, and in poorly resourced communities and countries.
Risk factors for scabies, particularly in developing countries, include:
- Crowded conditions
- Poor hygiene
- Poverty
- Malnutrition
- Homelessness
- Immunodeficiency.
In developed countries, scabies occurs in family outbreaks and children may acquire it from close play contact in school or sleepovers. In situations where there may be close physical contact for the delivery of personal care, such as in care homes, large outbreaks are not uncommon. In young adults, sexual spread is frequent.
What causes scabies?
Scabies infection is usually transmitted through close bodily skin contact such as holding hands for prolonged periods; spread amongst sexual partners is common. A brief handshake or hug does not usually allow for transmission unless the patient has crusted scabies.
Spread via fomites (clothing, towels, etc.) is very uncommon as the mite perishes within hours of leaving the host; it is relevant in crusted scabies.
Scabies cycle
- The smaller male mite fertilises the female on the surface of the skin and dies shortly after mating.
- The female mite burrows into the stratum corneum of the host where they lay 2 to 3 eggs per day.
- The female continues to burrow at a rate of 0.5 to 5mm per day for the duration of its 4 to 8-week lifespan.
- Eggs are deposited in the burrow and hatch into larvae after approximately 2 to 5 days.
- Hatched larvae mature into adult scabies mites in about 3 weeks. They migrate to the skin surface, and the cycle continues.
- The itchy rash is the result of a TH1-mediated hypersensitivity reaction to various mite-related antigens and is thus delayed.
What are the clinical features of scabies?
Infection typically presents with a classical itchy rash. Lesions are symmetrical, and mainly affect the hands, wrists, axillae, thighs, buttocks, waist, soles of the feet, areola and vulva in females and penis and scrotum in males. The neck and above are usually spared, except in cases of crusted scabies and in infections occurring in infants, the elderly, and the immunocompromised.
However, the rash may be generalised and eczematous features may dominate and mask the classical signs. Clinical suspicion is paramount.
Itch
- Generalised
- Occurs in 4 to 6 weeks following initial infection (during which time the host is infectious)
- Occurs within hours of subsequent re-infection
- Worse at night-time
- May persist for several weeks after completion of treatment.
Rash
- Erythematous papules
- Excoriations
- Linear scratch marks
- Dermatitis
- Nodules which may be skin coloured, red-brown, or violaceous
- Crusting (hyperkeratosis as seen in crusted scabies)
- Vesicles which may also be secondary to a superimposed bacterial infection.
Pathognomonic features which can assist in diagnosis
Burrows
- Curvilinear or serpiginous thread-like tracks measuring around 5–10 mm — these can be subtle
- Typically identified in the web spaces, palms, soles, fingers, toes, inner wrists, elbows, umbilicus, and beltline.
Nodules
- Varying in size between 3 and 15 mm
- May develop on the penis and scrotum in men
- On the upper thighs and gluteal folds
- Around the areolae in women
- In the axillae

A scabies burrow on the toe

A burrow on the palm - the mite can just be seen adjacent to the vesicle

Numerous palmar scabies burrows in an elderly lady

Scabies burrows on the palm

Scabies burrows on a babies foot

Interdigital scaling in the first web space of the hand
Crusted scabies
This variant occurs in the elderly and immunosuppressed – the palms and soles become covered in crusted plaques. There is massive infestation with mites, numbering in the thousands; it is highly infectious and there may be heavy infestation of bedding and upholstery.

Thick crusted plaques on the thumb and palm due to crusted scabies in an elderly woman
Secondary eruption
This can be a widespread nonspecific eczematous eruption on the torso and limbs and may partially obliterate the primary pathognomonic features.
How do clinical features vary in differing types of skin?
Scabies may present as granulomatous nodules in an infected person with a darker skin type.
Inflammatory changes appear as redness in white skin and greyness in black skin.
What are the complications of scabies?
Crusted scabies
- Previously known as Norwegian Scabies.
- Associated with dense hyperkeratosis of the skin.
- Caused by an altered host immune response.
- Seen particularly in patients with:
- Reduced T-cell immunity e.g., HIV
- Reduced peripheral sensation e.g., leprosy
- Patients unable to debride mites mechanically e.g., Down syndrome and subungual hyperkeratosis.
- Results in uncontrolled proliferation of mites (thousands to millions of mites, compared to 10–15 seen in classical scabies).
Bullous scabies
- Usually seen in elderly males.
- Bullae may be tense or flaccid.
- Thought to be due to either secondary infection of a scabetic lesion with Staphylococcus aureus or due to an autoantibody response.
Nodular scabies
- May be due to a local hypersensitivity reaction to dead mites or may be secondary to persistent infection.
- Commonly affects male genitalia (may be a widespread dominant feature in children) and breasts.
- Can be seen around the axillae or on the buttocks.
- May persist for months despite otherwise successful scabies treatment.
Other complications of classical scabies include:
Scabies incognito
- Modification of the clinical picture secondary to inappropriate use of steroids after misdiagnosis.
- Results in delayed diagnosis, sometimes for months or even years.
Secondary bacterial infection
- Staphylococcus aureus or Streptococcus pyogenes bacteraemia.
- Impetigo.
- Pustular lesions on the palms, soles, fingers, and toes.
- Toxin-mediated diseases such as toxic shock syndrome, glomerulonephritis, and acute rheumatic fever.
Psychological distress
- Scabies often afflicts young adults living away from home for the first time and the development of a contagious rash can be embarrassing. Stigma can lead to an inability to ensure household or sexual contacts are treated.
- Sleep disturbance and an unsightly rash compound the emotional impact of the illness, especially where diagnosis and comprehensive treatment is delayed, when the symptoms can persist for many months.

Scabies with superadded streptococcal infection

Scabies nodules in the axilla

Axillary scabies nodules in an infant
How is scabies diagnosed?
A high index of suspicion should be used when assessing a patient with a new widespread itchy rash, especially one who reports itchy close contacts. The diagnosis is typically clinical and most easily confirmed using dermoscopy.
Several invasive and non-invasive tests exist to aid in confirming a diagnosis of scabies:
- Dermoscopy may reveal the ‘delta wing jet’ or ‘mini triangle’ sign. In crusted scabies, dermoscopy may show hyperkeratosis.
- For information on trichoscopic findings in scabies of the scalp, see Trichoscopy of scalp infestations.
- Skin scrapings using either a blade or needle allow direct visualisation of mites eggs or mite faeces on microscopy. Visualisation of a live mite by the patient galvanises treatment concordance.
- A burrow ink test may reveal a classical zig-zag line where the ink has tracked into a burrow.
- Adhesive tape test is used to transfer a sample from a suspicious lesion directly to a microscope slide.
- Skin biopsy, although rarely necessary, will show eggs, larvae, faeces, and mites.
It is useful to examine close contacts in suspicious cases as pathognomonic signs are often seen in those with minimal symptoms.
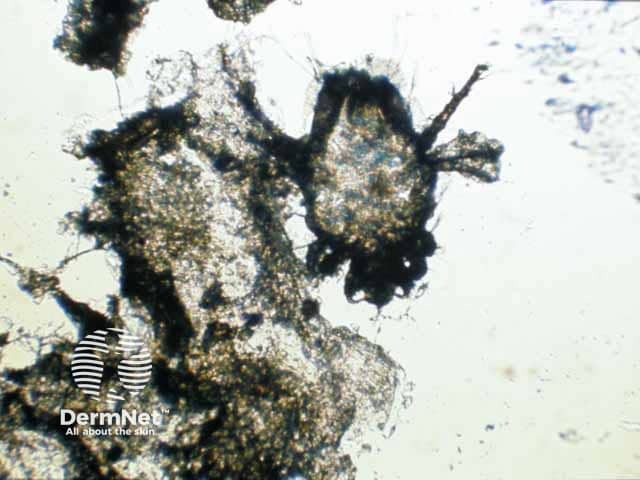
A scabies mite on microscopy after extraction from a burrow
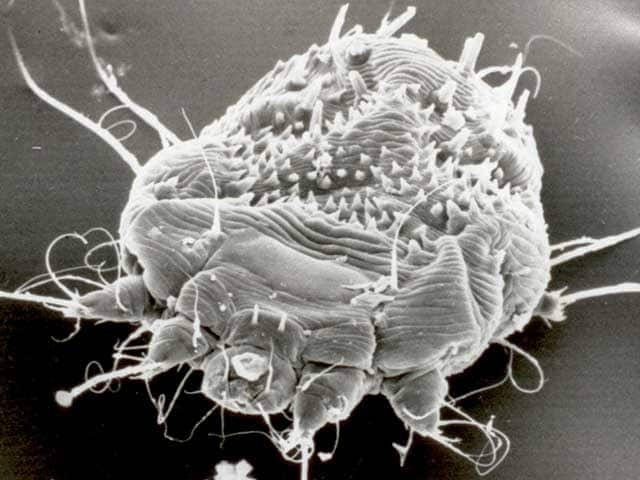
Scanning electron microscopy of Sarcoptes scabei
The International Alliance for the Control of Scabies (IACS) updated consensus criteria for the diagnosis of scabies in 2020, copied below:
A: Confirmed scabies is diagnosed if there is at least one of:
- A1: Mites, eggs or faeces on light microscopy of skin samples
- A2: Mites, eggs or faeces visualized on an individual using a high-powered imaging device
- A3: Mite visualised on an individual using dermoscopy.
B: Clinical scabies is diagnosed if there is at least one of:
- B1: Scabies burrows
- B2: Typical lesions affecting male genitalia
- B3: Typical lesions in a typical distribution and two history features.
C: Suspected scabies is diagnosed if there is one of:
- C1: Typical lesions in a typical distribution and one history feature
- C2: Atypical lesions or atypical distribution and two history features.
History features are:
- H1: Itch
- H2: Positive contact history with an individual who has an itch or typical lesions in a typical distribution.
Notes
- These criteria should be used in conjunction with the full explanatory notes and definitions (in preparation by IACS).
- Diagnosis can be made at one of the three levels (A, B or C).
- A diagnosis of clinical and suspected scabies should only be made if other differential diagnoses (such as eczema and impetigo) are considered less likely than scabies.
What is the differential diagnosis for scabies?
- Bullous skin disorders
- Dermatitis
- Folliculitis
- Papular urticaria
- Prurigo (subacute)
- Psoriasis
- Infantile acropustulosis
What is the treatment for scabies?
General measures
- Launder sheets, towels, and clothes worn recently. Outer garments, duvets, and blankets should be aired for 72 hours.
- Vacuum soft furnishings where possible, although this may be of limited benefit.
- Clip nails and clean any subungual debris.
Specific measures
It is important to note that all close contacts of a confirmed case of scabies should complete eradication therapy, whether they are symptomatic or not. Contacts may be infected but asymptomatic for several weeks, therefore they may continue to infect others and even reinfect the index case.
Topical therapies
- Topical 5% permethrin (acaricidal and ovicidal) cream or lotion remains first-line therapy.
- Applied over the whole body including face, neck, scalp and ears (or as otherwise advised) and left overnight for 8–12 hours. Reapplication is needed if hands are washed during the treatment period.
- Application should include under the nails and between the toes.
- Treatment should be repeated after 7–10 days.
- If the case is permethrin-resistant, or permethrin is not available, alternative insecticides, include 10–25% benzyl benzoate or 0.5% malathion aqueous lotion.
- Spinosad is a topical horticultural insecticide and is effective against scabies where it is available.
Oral therapies
- Oral ivermectin is indicated in cases of topical failure, inability to comply with topical therapy, non-adherence to topical therapy, institutional outbreaks, mass treatment of populations, and crusted scabies.
- Repeat dose after 2 weeks.
- Latest data suggests oral ivermectin is equally as effective as topical 5% permethrin cream or lotion, however may be slower-acting.
- According to French dermatology guidance (2024), ivermectin may be an option for children over the age of 2 months. It can also be used in breastfeeding women and during pregnancy from the second trimester onwards, if topical therapies have proved ineffective.
- Oral moxidectin is as yet unlicensed, but an effective agent that has good skin retention — it may be effective as a single treatment and prevent re-infestation.
Practical advice to patients
- Provide written instruction.
- Explain the necessity for complete, contemporaneous compliance with topical therapy.
- Household members should elect an early, convenient evening on which to be treated, assemble bedding and clothing for laundry, and apply the topical treatment before dressing and remaking beds.
- Itching may last for several weeks, and this does not represent persistent infection or treatment failure.
Post-scabetic itch
- May persist for weeks
- Moderate potency topical steroids may be used and required for 3–4 weeks, particularly if the patient has a widespread eczematous reaction
- Antihistamines are helpful in some cases
- Emollient use and soap avoidance should be advised
- Persistent nodules may need potent topical or intralesional steroids.
Scabies and pregnancy
- 5% permethrin cream or lotion is considered safe in pregnancy and while lactating.
- Alternative topical preparations include sulphur 5–10% cream, ointment, or lotion.
- Oral ivermectin is not advised during pregnancy.
What is the outcome for scabies?
Classical scabies is associated with a good prognosis provided compliance is satisfactory and all close contacts (symptomatic or not) are simultaneously treated. Crusted scabies may need prolonged and repeated treatment and patients may have significant underlying conditions that will influence the prognosis. Pyococcal infection of scabies is one of the most common causes of acute glomerulonephritis globally.
Scabies reinfection is common and is usually secondary to spread from untreated close contacts. Repetitive use of disinfectants can lead to irritant dermatitis, and in the mistaken belief of continued scabies infestation, yet more disinfectant is used.
Bibliography
- Arora P, Rudnicka L, Sar-Pomian M, et al. Scabies: A comprehensive review and current perspectives. Dermatol Ther. 2020;33(4):e13746. doi:10.1111/dth.13746. Review
- Engelman D, Yoshizumi J, Hay RJ, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol. 2020;183(5):808–20. doi:10.1111/bjd.18943. Journal
- Leung AKC, Lam JM, Leong KF. Scabies: A Neglected Global Disease. Curr Pediatr Rev. 2020;16(1):33–42. doi:10.2174/1573396315666190717114131. Review
- Morand A, Weill A, Miquel J, et al. Management of scabies in children under 15 kg and pregnant or breastfeeding women: recommendations supported by the Centre of Evidence of the French Society of Dermatology. Br J Dermatol. 2024;191(6):1014–6. PubMed
- Richards RN. Scabies: Diagnostic and Therapeutic Update. J Cutan Med Surg. 2021;25(1):95–101. doi:10.1177/1203475420960446. Journal
- Seiler JC, Keech RC, Aker JL, Miller W, Belcher C, Mettert KW. Spinosad at 0.9% in the treatment of scabies: Efficacy results from 2 multicenter, randomized, double-blind, vehicle-controlled studies. J Am Acad Dermatol. 2022;86(1):97–103. doi:10.1016/j.jaad.2021.07.074. PubMed
On DermNet
- Arthropod infestations
- Crusted scabies
- Crusted scabies pathology
- Differential diagnosis of very itchy skin
- Insecticides and the skin
- Institutional scabies
- Ivermectin
- Scabies images
- Scabies pathology
- Trichoscopy of scalp infestations
Other websites
- Scabies — British Association of Dermatologists
- The International Alliance for the Control of Scabies (IACS)
