Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Olivia Kuo, Addenbrookes Hospital, Cambridge, United Kingdom, March 2022; minor update September 2024.
Previous contributors: A/Prof Amanda Oakley, Dermatologist; Vanessa Ngan, Staff Writer, New Zealand, 2014. Copy edited by Gus Mitchell.
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Rosacea is a chronic inflammatory skin condition predominantly affecting the central face and most often starts between the age of 30–60 years.
Rosacea is common and is characterised by persistent facial redness. It typically has a relapsing and remitting course, with symptoms controlled by lifestyle measures, general skin care, medications, and procedural interventions.

Papulopustular rosacea on the cheeks

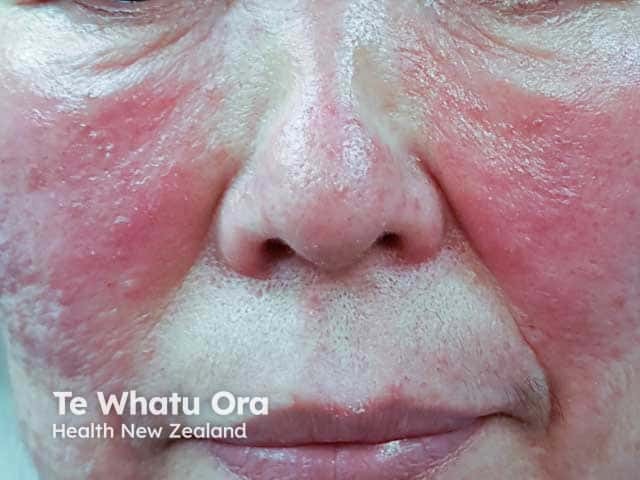
Erythematotelangiectatic and papulopustular rosacea on the cheeks

Papular rosacea on the cheeks

Telangiectatic vessels in a rinophyma shown on dermoscopy (RO-patient4)

Rhinophyma and papular rosacea on the chin (RO-patient2)

Papulopustular and ocular rosacea
Click here for more images of rosacea
Rosacea is estimated to affect around 5% of adults worldwide. Although rosacea is often thought to affect women more than men, studies have revealed an approximately equal gender distribution.
Rosacea typically presents after the age of 30 and becomes more prevalent with age. However, it can occur at any age and occasionally presents in children. Although rosacea can affect anyone, it is more common in those with fair skin, blue eyes, and those of Celtic or North European descent. It may be more difficult and under-recognised in patients with skin of colour.
Rosacea has been associated with depression, hypertension, cardiovascular diseases, anxiety disorder, dyslipidemia, diabetes mellitus, migraine, rheumatoid arthritis, Helicobacter pylori infection, ulcerative colitis, and dementia.
The pathogenesis of rosacea is thought to be multifactorial and includes:
The most significant environmental trigger is UV radiation; affected skin is more sensitive to exposure. UV radiation can damage the dermis and increase skin inflammation.
Cutaneous features include:
Transient recurrent erythema, ie, flushing
Inflammatory papules and pustules (papulopustular)
Phymatous changes

Rhinophyma

Rhinophyma showing swelling and sebeceous gland openings (RO-patient1)

Steroid induced papulopustular rosacea

Steroid induced rosacea on the forehead

Steroid induced facial rosacea

Steroid induced papular rosacea
Swelling and papulopustules in steroid induced rosacea (SR-patient4)
Occasionally rosacea induces facial lymphoedema (Morbihan disease), producing redness, and swelling of the face and lids.
Facial tenderness and burning pain accompanied by redness and flushing (neurogenic rosacea) is a rare variant of rosacea.

Lid lymphoedema and glabellar swelling in Morbihan disease

Violaceous swelling of the lower lids in Morbihan disease
Non-cutaneous ocular features (affects over 50% of patients with rosacea):
Click here for images of rosacea
Rosacea is diagnosed more frequently in fair-skinned patients of Celtic and Northern European descent.
It may be harder to identify key features of rosacea in patients with skin of colour. These features are likely under-recognised and rosacea may be underdiagnosed in these patients.
Complications of rosacea include:
Rosacea is diagnosed clinically in the majority of cases. Diagnosis is made according to diagnostic and major criteria recommended by the 2017 global ROSacea COnsensus (ROSCO) panel. This requires one diagnostic criterion or two major criteria to be fulfilled.
In patients with darker phototypes where erythema and telangiectasia (visible blood vessels) is more difficult to visualise, greater emphasis may be placed on other major and minor features.
In cases where there is diagnostic uncertainty, skin biopsy may be considered.
Other conditions that could present with similar cutaneous features include:
Although there is no cure for rosacea, symptoms can be managed with the following lifestyle measures, medical, and procedural interventions.
All patients with rosacea should receive education on general skincare and lifestyle measures.
Existing treatments for rosacea can be very effective — however, they often target only one feature. This means that a combination of therapies are required where patients present with multiple features and in severe rosacea.
Many of the following treatments are first-line therapies recommended by the 2019 ROSCO panel:
For more information, see Ocular rosacea.
Although rosacea is not a life-threatening condition, it is a chronic disease that requires long-term management of relapsing and remitting symptoms. Complete resolution of clinical features has been shown to prolong time to symptom relapse and have greater positive impact on quality of life compared with incomplete resolution.