Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Mycosis fungoides palmaris et plantaris — extra information
Mycosis fungoides palmaris et plantaris
Author: Dr Karen Koch, Consultant Dermatologist, Wits University Donald Gordon Medical Centre, Johannesburg, South Africa. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. April 2019.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
What is mycosis fungoides palmaris et plantaris?
Mycosis fungoides palmaris et plantaris is a very rare localised form of mycosis fungoides, a type of cutaneous T-cell lymphoma. While mycosis fungoides affects the hands in about 10% of cases, the palmoplantar variant only affects the hands and feet [1].
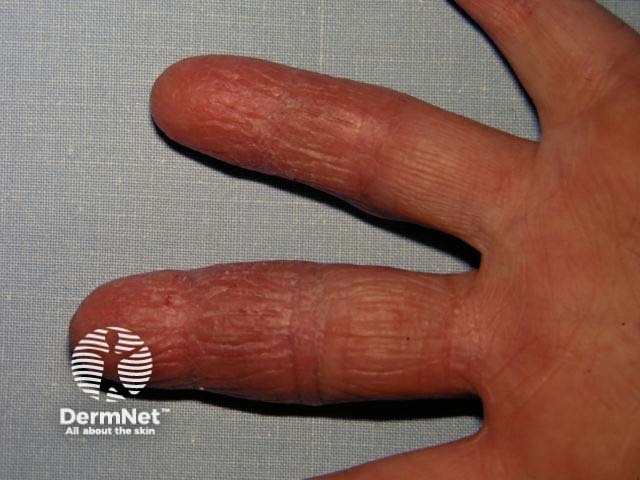
Mycosis fungoides palmaris

Mycosis fungoides palmaris

Mycosis fungoides of the palms
Who gets mycosis fungoides palmaris et plantaris?
There are fewer than 30 reported cases of mycosis fungoides palmaris et plantaris. Although mycosis fungoides palmaris et plantaris can affect all ages, it tends to occur in middle-aged adults [2]. It affects men more frequently than women [2].
What causes mycosis fungoides palmaris et plantaris?
The exact cause of mycosis fungoides palmaris et plantaris is not known. No single viral, genetic, epigenetic, or environmental factor has been linked to mycosis fungoides [3].
What are the clinical features of mycosis fungoides palmaris et plantaris?
Mycosis fungoides palmaris et plantaris most often resembles persistent hand eczema and foot eczema [1,2].
- It may affect only the hands, only the feet, or both hands and feet.
- The palms and soles are more often affected than the tops of the hands and feet.
- It presents with thickened scaly red plaques, which may or may not be itchy.
- The plaques tend to persist or relapse despite treatment.
However, the clinical features of mycosis fungoides palmaris et plantaris can be widely variable. Blisters and pustules, erosions, tumours, and ulcers have all been reported. It rarely affects the nails [2].
What are the complications of mycosis fungoides palmaris et plantaris?
Mycosis fungoides palmaris et plantaris may cause pain, fissuring, and difficulty in using the hands and feet.
- Secondary bacterial infection (staphylococci and/or streptococci) can result in pustules, crusting, and pain.
- Progression to a more extensive form of cutaneous T-cell lymphoma or Sézary syndrome has not been reported, but this remains a potential complication.
How is mycosis fungoides palmaris et plantaris diagnosed?
The clinician may be alerted to an unusual cause of hand and foot dermatitis by frequent relapses and a resistance to regular treatments. A full skin examination should be undertaken, including evaluation of the lymph nodes, as enlarged lymph nodes could suggest a more widespread lymphoma.
The diagnosis of mycosis fungoides palmaris et plantaris is established by a skin biopsy and assessment by a dermatopathologist.
The histological features of mycosis fungoides can be subtle, as early T-cell lymphoma may resemble eczema. Several repeated biopsies may be necessary.
A blood count is needed to ensure there is no associated Sézary syndrome.
What is the differential diagnosis for mycosis fungoides palmaris et plantaris?
The differential diagnosis for mycosis fungoides palmaris et plantaris includes all forms of hand dermatitis. The following should be considered:
- Contact dermatitis — hand eczema caused by exposure to harsh chemicals/irritants or allergens; this rarely affects the feet
- Pompholyx — a form of eczema in which there are itchy clusters of blisters along the sides of the fingers and on the palms, that may be exacerbated by sweating; pompholyx can also affect the feet.
- Palmoplantar psoriasis — thickening, scaling, and flaking of the hands and feet; psoriatic nail dystrophy may be observed
- Palmoplantar pustulosis — a chronic disorder characterised by persistent tender groups of pustules on the palms and soles
- Mycosis fungoides — the usual, more widespread form of cutaneous T-cell lymphoma, which presents as eczematous patches, plaques, nodules, tumours, and ulcers, generally in sun-protected areas, such as the trunk; the rash is not limited to the hands and feet.
What is the treatment for mycosis fungoides palmaris et plantaris?
Treatment options for mycosis fungoides palmaris et plantaris depend on the extent of disease, local expertise, and the available drugs and equipment. The following have been used alone or in combination with success:
- Topical steroids
- Ultraviolet B (UVB) phototherapy
- Psoralen and ultraviolet A (PUVA) photochemotherapy
- Bexarotene gel (a topical rexinoid)
- Topical nitrogen mustard
- Chemotherapy
- Localised radiotherapy or electron beam therapy
- Oral retinoids
- Methotrexate.
What is the outcome for mycosis fungoides palmaris et plantaris?
Mycosis fungoides palmaris et plantaris very rarely spreads to other tissues and is considered to be slow-growing.
Unlike some other lymphomas, the outlook is generally good. Symptoms can usually be controlled with treatment. However, treatment is not curative, and it may recur after a remission lasting many months or years.
References
- Resnik KS, Kantor GR, Lessin SR, et al. Mycosis fungoides palmaris et plantaris. Arch Dermatol 1995; 131: 1052–6. PubMed
- Nakai N, Hagura A, Yamazato S, Katoh N. Mycosis fungoides palmaris et plantaris successfully treated with radiotherapy: case report and mini-review of the published work. J Dermatol 2014; 41: 63–7. DOI: 10.1111/1346-8138.12308. PubMed
- Wong HK, Mishra A, Hake T, Porcu P. Evolving insights in the pathogenesis and therapy of cutaneous T-cell lymphoma (mycosis fungoides and Sezary syndrome). Br J Haematol 2011; 155: 150–66. DOI: 10.1111/j.1365-2141.2011.08852.x. PubMed
On DermNet
- Cutaneous T-cell lymphoma
- Sézary syndrome
- Mycosis fungoides pathology
- Cutaneous T-cell lymphoma images
- Cutaneous B-cell lymphoma
- Indolent cutaneous CD8+ lymphoid proliferation pathology
- Leukaemia cutis
- Electron beam radiation for cutaneous lymphoma
- Skin manifestations of haematological diseases
Other websites
- Cutaneous Lymphoma Foundation — A US-based patient support, advocacy, and research organisation
- Leukaemia & Blood Foundation New Zealand — a New Zealand-based patient support, advocacy, and research organisation
- Mycosis fungoides — British Association of Dermatologists [patient information leaflet]
- Cutaneous T-cell lymphoma — Medscape
