Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Tae Yeb (Terry) Kim, House Officer, North Shore Hospital, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell. April 2020.
Introduction Demographics Causes Clinical features Complications Diagnosis Differential diagnoses Treatment Outcome
CLOVES syndrome is a rare, progressive congenital disorder that involves multiple organs including the skin, the vascular system, and the musculoskeletal system [1].
CLOVES is a mnemonic acronym for:
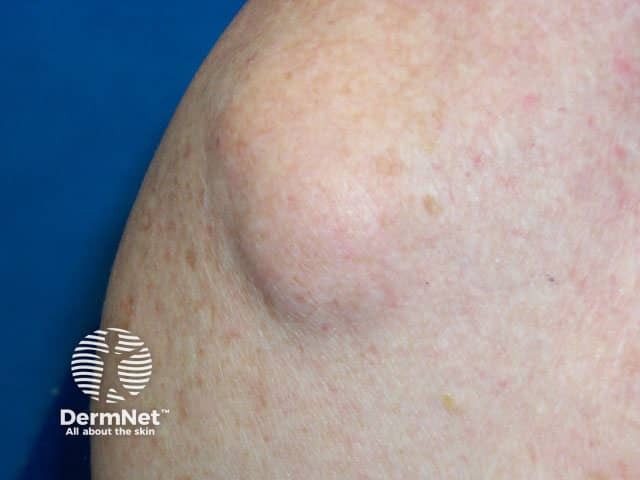
Lipoma


Verrucous epidermal naevus
Note: images are not from patients with CLOVES syndrome.
CLOVES syndrome is rare and there is no accurate estimation of the incidence or prevalence globally. The mutation is sporadic and there is no known familial predisposition.
CLOVES syndrome is caused by a somatic mosaic gain-of-function mutation (a mutation that occurs after the creation of the zygote) in the PIK3CA gene [2]. It is a part of the PIK3CA-Related Overgrowth Spectrum (PROS), a group of rare overgrowth disorders [3].
CLOVES syndrome presents at birth with vascular malformations, adipose tissue overgrowth (lipomas), epidermal naevi, and varying degrees of bony deformities [4]. Asymmetrical, disproportionate growth may be evident in prenatal scans [5].
The characteristic features of CLOVES syndrome include:
The complications of CLOVES syndrome depend on its extent. These can include:
The diagnosis of CLOVES syndrome is based upon:
Radiological findings can support the diagnosis. Vascular malformations and lipomatous masses can be assessed by magnetic resonance imaging (MRI) [11].
CLOVES has most commonly been misdiagnosed as proteus syndrome, which is distinguished by the normal appearance at birth, the progression, distortion and body overgrowth with age, and the characteristic connective tissue naevi [12].
Other differential diagnoses for CLOVES syndrome may include:
There is no cure for CLOVES syndrome. Improvement has been reported from experimental treatments with:
The prognosis of CLOVES syndrome is usually poor, due to its complications. However, there are indications that treatments with PIK3CA inhibitors will prove effective.