Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Systemic diseases Pigmentary disorders
Last Reviewed: March, 2025
Authors: Dr. James A. Ida, MD, MS, Dermatologist, Veterans Administration, USA (2025)
Previous authors: Vanessa Ngan, DermNet Staff writer (2004); Abdullah Haroon, University of Ottawa, (2024)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet Content Department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
Acanthosis nigricans is a skin condition characterised by a velvety papillomatous overgrowth of the epidermis. Darkening and thickening (epidermal hyperplasia) of the skin occurs mainly in the flexural areas, particularly the axillae, groin, inframammary region, and neck.
Acanthosis nigricans (AN) is usually a sign of an underlying metabolic or hormonal condition or disease, such as obesity or diabetes (most commonly type 2 diabetes but also reported in type 1 diabetes, particularly when associated with obesity). It may also be associated with certain drugs, such as systemic glucocorticoids or oral contraceptives. Its presence as a sign of internal malignancy (malignant AN) is very rare.
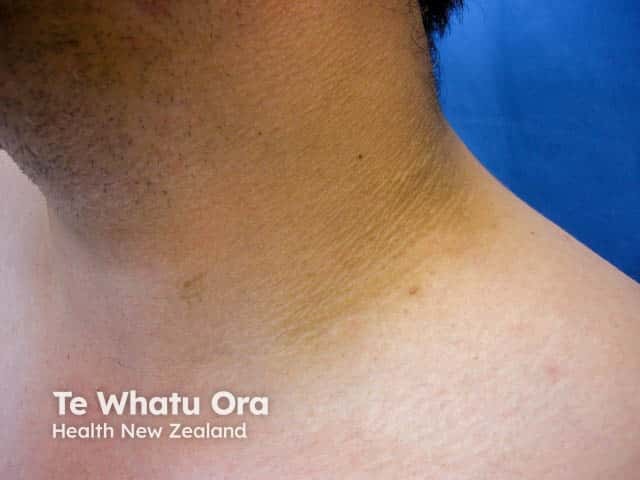
Acanthosis nigricans on the neck

Axillary acanthosis nigricans

Acanthosis nigricans
The exact cause of AN is still unclear. However, it is predominantly linked to states of insulin resistance (IR) wherein obesity, diabetes, and/or other metabolic disorders (eg, metabolic syndrome, polycystic ovary syndrome, and generalised lipodystrophy) co-exist. Insulin in high concentrations has been shown to cross the dermal-epidermal junction, and in high concentrations to have growth-stimulating effects through its binding to type 1 insulin-like growth factor receptor (IGFR) on keratinocytes. It is this activation of IGFR that stimulates the proliferation of keratinocytes and leads to AN.
Other less common presentations of AN include:
A recently described presentation of AN-like lesions among darker-skinned individuals, involving the forehead, cheeks, including the malar areas, and fingers was also found to be strongly associated with obesity and metabolic disorders.
Malignant AN is a rare paraneoplastic syndrome likely due to the release of stimulatory growth factors by tumour cells and is typically associated with gastrointestinal malignancies, especially gastric adenocarcinoma (60%); other associated cancers include hepatobiliary carcinoma, squamous cell carcinoma, malignant melanoma, and Wilms tumour. The oral cavity is involved in 25–50% of cases.
Tripe palms are a variant of malignant AN with a 90% association with internal malignancy.
Acanthosis nigricans is characterised by symmetric, thickened, brown, velvety patches and plaques that appear most commonly in the intertriginous areas (ie, the axillae, groin, and back and sides of the neck). In women, the nipples and areolae of the breasts, the vulva, and the perineum may also be involved. The lesions of AN may become macerated and malodorous, and skin tags are an additional frequent finding.
Lesions affecting the mucosal surfaces of the oral cavity, nose, larynx, and oesophagus tend to be more common and more extensive in malignant acanthosis nigricans as does the finding of pruritus. Pruritus may be present and is very common in malignant acanthosis nigricans.
The mainstay for treatment is to manage the underlying disease. Patient education is also an important component.
Treatment of acanthosis nigricans can also be undertaken for cosmetic reasons. Towards this end, some pharmacologic modalities include:
Procedural modalities include:
Outcomes depend on the cause. Acanthosis nigricans may be a vital marker of underlying conditions which themselves carry significant risk to overall morbidity and mortality, such as obesity, metabolic syndrome, diabetes, and even serious internal malignancies.
Outcomes naturally depend on the underlying cause of the AN. If the underlying etiology can be addressed, such as through weight loss interventions, then the acanthosis nigricans is expected to improve or fully resolve. Obesity, metabolic syndrome, and diabetes have deleterious effects on overall morbidity and mortality. Hereditary acanthosis nigricans may stabilise or even regress spontaneously in some cases. Malignant acanthosis nigricans, however, is associated with a poor prognosis, with an average survival time of two years from diagnosis of the AN due to mortality from advanced underlying malignancy.