Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Last Reviewed: August, 2025
Authors: Dr Sam Hughes, Dermatology Registrar, St John’s Institute of Dermatology, London, England; Dr Xi Hui Felicia Chan, Medical Registrar, Te Whatu Ora Waikato, New Zealand (2025)
Peer reviewed by: Nancy Huang (MBChB), Dermnet Medical Writer, New Zealand (2025)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outcome
Parry-Romberg syndrome (PRS) is a rare acquired disorder characterised by the progressive atrophy of skin, fat, muscle, bone, and cartilage typically on one side of the face. Systemic manifestations may occur, particularly with neurologic and ophthalmic involvement.
This disorder is considered by some to be a rare, severe variant of linear morphoea (localised scleroderma).
Other names for Parry-Romberg syndrome include:
Hemiatrophy of the tongue in addition to facial changes of fat and muscle atrophy (PRS-patient2)

Dermal sclerosis is evident in morphoea, but there was also cerebral and lingual changes more in keeping with PRS (PRS-patient1)
Parry-Romberg syndrome classically presents within the first two decades of life, however cases have also been reported in older adults. PRS can affect both genders, but is more commonly seen in females. PRS does not appear to show any racial predilection.
The cause of PRS is unknown (idiopathic). Several factors have been proposed to play a role in the pathogenesis of PRS.
Common etiological theories include:
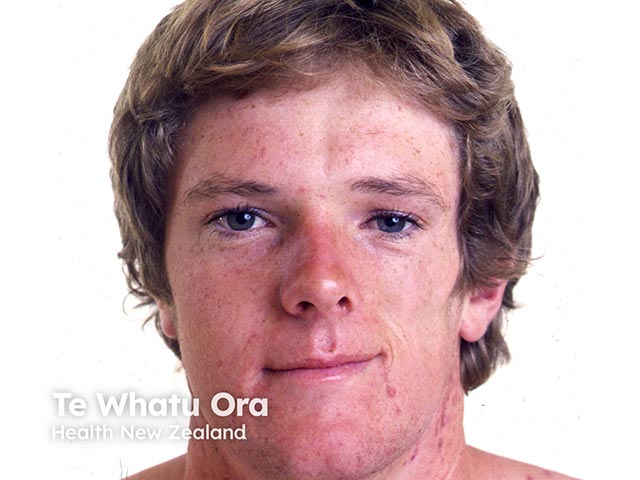
Parry-Romberg syndrome is characterised by the unilateral wasting of facial skin, fat, muscles, cartilage, bones, or even glands. This creates a sunken, indented appearance of one side of the face. The severity and speed of atrophy vary greatly from patient to patient.
In rare cases, bilateral facial involvement can occur, or other parts of the body can be affected (eg, torso and extremities).
Additional facial features:
Parry-Romberg syndrome can also cause extracutaneous manifestations; an estimated 15% of patients have neurologic involvement, and up to 35% have ophthalmic involvement.
Neurologic features:
Ophthalmic features:
There are no notable differences in presentation based on skin type.
There are currently no universally accepted diagnostic criteria. Parry-Romberg syndrome is primarily a clinical diagnosis, based on the history of a slowly progressive, localised, hemifacial atrophy, and the exclusion of other causes.
Neuroimaging with CT/MRI should be performed if patients have neurological symptoms; they may also aid the diagnosis by demonstrating changes such as lipoatrophy. Seizures should prompt evaluation with electroencephalogram studies.
Although histopathology is not required for diagnosis, skin biopsy reveals minimal sclerosis, extensive dermal fat atrophy, preservation of dermal elastic tissue, and a decrease in adnexal structures.
Other causes of acquired localised lipoatrophy:
Currently, there is no known cure or standardised treatment for Parry-Romberg syndrome. Instead, efforts are aimed at halting disease progression and treating acute complications. Once the disease has stabilised, aesthetic rehabilitation may be initiated.
Treatment of Parry-Romberg syndrome requires a multidisciplinary approach and may involve dermatologists, neurologists, ophthalmologists, plastic surgeons, maxillofacial surgeons, and dentists.
Treatments to halt disease activity are similar to those employed for scleroderma and involve immunosuppression or immunomodulation:
There is no known way of preventing Parry-Romberg syndrome.
Parry-Romberg syndrome is an incurable disease that tends to slowly progress over a 2 to 20-year period, before spontaneously entering a stable phase where disease progression halts. Prognosis is favourable and patients are expected to have a normal life expectancy.
Mild cases of Parry-Romberg syndrome usually do not cause disability other than cosmetic effects.