Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Dr Hamish Wu, Medical Registrar, Auckland; and Honorary Associate Professor Paul Jarrett, Dermatologist, Middlemore Hospital and The University of Auckland, New Zealand (2023)
Previous contributors: Dr Mark Duffill, Dermatologist (2008)
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction Demographics Causes Clinical features Variation in skin types Complications Diagnosis Differential diagnoses Treatment Outcome
Relapsing polychondritis is a rare autoimmune disorder characterised by recurrent episodes of inflammation and destruction of cartilaginous tissues.
Relapsing polychondritis most commonly affects the cartilage in the ears, nose, trachea, and joints, causing pain, swelling, and stiffness. The eyes, heart, and blood vessels are less commonly affected but can result in serious complications.
While there is no clear aetiology or specific diagnostic test for relapsing polychondritis, early recognition and treatment improve prognosis.

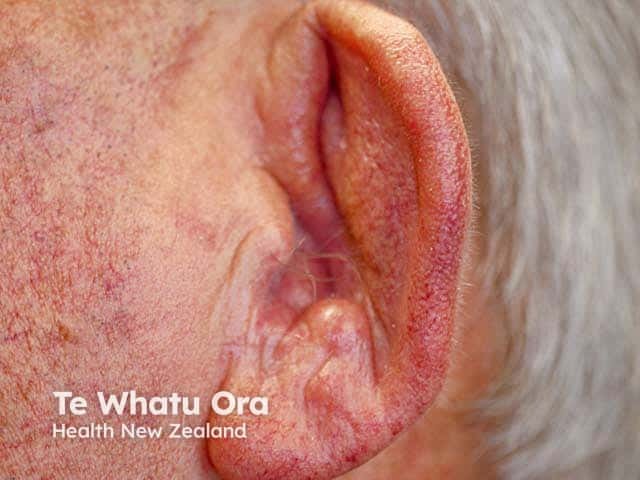
A swollen red inflammed pinna due to polychondritis - both ears were affected. Note sparing of the non-cartilaginous lobe (RP-patient1)

Swelling and erythema of the upper cartilaginous part of the helix with sparing of the non-cartilaginous lobe

Red eyes (which can be due to scleritis, episcleritis, conjunctivitis, and iritis) seen as part of the presentation of relapsing polychondritis (RP-patient1)
Collapsed cartilage in polychondritis
Xray of auricular relapsing polychondritis
See more images of relapsing polychondritis
Relapsing polychondritis most commonly presents as inflammation of the cartilage of the ears (auricular chondritis) and nose (nasal chondritis).
See images of relapsing polychondritis
Erythema of inflamed cartilage may be less evident in darker skin phototypes.
Diagnosis can be challenging as relapsing polychondritis mimics other conditions. Diagnosis is often determined using a combination of clinical features, imaging, and laboratory results.
The McAdam’s diagnostic criteria require at least 3 of the following (and usually a tissue biopsy consistent with chondritis as well):
Alternative diagnostic criteria are also specified in the modified (Damiani) criteria; if the above criteria are not satisfied, diagnosis could also be made on the basis of:
There is no known cure for relapsing polychondritis. Treatment aims to control symptoms and prevent complications.
Other immunosuppressive agents used include:
In severe cases, surgical interventions such as a tracheostomy, nasal septal repair, bronchial segment repair, or cardiac valve replacement may be necessary.
Relapsing polychondritis has a variable prognosis depending on the severity and the degree of organ involvement. Early diagnosis and treatment can improve outcomes and prevent complications.
In general, the mortality rate is believed to be ~5–10%. Respiratory failure is a major cause of death. Patients with cardiovascular or renal dysfunction have poorer outcomes.