Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Jen Taylor, Dermatology Registrar, Waikato Hospital, Hamilton, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Hamilton, NZ. Copy edited by Gus Mitchell. August 2018.
Introduction - cellulitis
Clinical features
Clinical conditions of cellulitis mimics
Cellulitis is an acute bacterial infection of the dermis and subcutaneous tissues of the skin. It is commonly caused by either Streptococcus pyogenes or Staphylococcus aureus. Cellulitis presents as an enlarging area of red, hot, swollen, and tender skin. Cellulitis can occur anywhere on the body but is most commonly seen on the lower leg. It may be accompanied by lymphangitis, which appears as a red streak following the lymphatic vessels towards the local lymph node (which may also be tender and enlarged).
Signs of cellulitis are nonspecific and the diagnosis rests largely on the patient's history and physical examination. A number of skin conditions may 'mimic' cellulitis, and around 30% of cases of cellulitis are misdiagnosed. Distinguishing between cellulitis and these mimicking conditions is important to avoid unnecessary treatment and complications, and to expedite appropriate treatment.



Cellulitis of the lower legs is almost always unilateral. Bilateral distribution of cellulitis only rarely occurs, usually as a result of an underlying condition, such as lymphoedema. The bilateral distribution of a rash in the absence of other symptoms of cellulitis should prompt a search for an alternative diagnosis.
If untreated, cellulitis will progress rapidly. If appropriate antibiotics are commenced, the cellulitis should respond within hours to days. A lack of response suggests an alternative diagnosis.
A patient with cellulitis may experience symptoms such as nausea and malaise.
Signs of infection from cellulitis include:
There may be a portal of entry, such as an ulcer or injury, that enables bacteria to breach the skin's defences. Other risk factors include chronic oedema, lymphoedema, obesity, and diabetes mellitus.
Other skin infections that share similar features to cellulitis are erysipelas, necrotising fasciitis, and herpes zoster.
Erysipelas is a superficial variant of cellulitis that is also caused predominantly by S. pyogenes or S. aureus.
Erysipelas presents with:



Necrotising fasciitis is a bacterial infection that affects the subcutaneous tissues. As it does not affect the epidermis and upper dermis, its features may be subtle in the early stage, but infection later gives rise to rapid and severe tissue necrosis if untreated. Most patients with necrotising fasciitis are seriously unwell with septic features.
Clues to the diagnosis of necrotising fasciitis include:

Necrotising fasciitis

Necrotising fasciitis

Necrotising fasciitis
Some of the symptoms of herpes zoster (shingles) are similar to cellulitis, including:
However, herpes zoster is characterised by its dermatomal distribution and umbilicated vesicles. Antibiotics are not effective against herpes zoster virus, which is treated with antiviral agents, such as aciclovir.

Herpes zoster

Herpes zoster

Herpes zoster
Venous disease of the lower legs affects around 20% of people aged over 70 years. Damage or degeneration of the leg veins is a very common reason for red legs. Signs of venous insufficiency may include:
These changes have been classified in a framework of symptoms known as the clinical, aetiological, anatomical and pathophysiological (CEAP) classification.
In this condition, dilated skin vessels result in a red, dusky discolouration of the legs when sitting or standing. Patients are typically asymptomatic.
Prolonged oedema leads to inflammation and subsequent redness, itch, dryness, and scaling and what is referred to as venous eczema. Venous eczema is not usually as red, hot, or oedematous as cellulitis.

Venous eczema

Venous eczema

Venous eczema
Superficial thrombophlebitis causes redness, heat, and tenderness resembling cellulitis, except that the inflammation is linear, following the course of the underlying thrombosed vein, which is palpable and tender. Oedema is absent and the skin is not taut, smooth, or shiny. There are no systemic symptoms.
The inflammation from deep venous thrombosis does not spread to the skin surface nor cause erythema.
Lipodermatosclerosis can be acute or chronic. Acute lipodermatosclerosis is often tender and bright red in colour, and occurs with or without oedema. Systemic symptoms and signs of infection are absent. Later, a reddish-brown discolouration indicates prolonged inflammation and deposition of haemosiderin (an insoluble form of iron that has leaked out of the swollen capillaries).
Chronic lipodermatosclerosis has a ‘tethered down’ appearance due to fibrosis (hardening) of the deeper tissues.

Acute lipodermatosclerosis

Acute lipodermatosclerosis

Chronic lipodermatosclerosis
Dermatitis, or eczema, describes a group of common inflammatory skin conditions. Leg dermatitis may be due to atopic dermatitis, discoid eczema, contact dermatitis, eczema craquelé (due to dry skin), or venous eczema. Combinations can occur.
Acute eczema can mimic cellulitis, regardless of the cause; it is characterised by erythema, weeping, crusting, and blistering and may be secondarily infected (impetiginisation).

Acute eczema

Acute eczema

Acute eczema
Contact dermatitis is classified as contact irritant dermatitis or contact allergic dermatitis (a type IV hypersensitivity reaction).
Irritants that cause contact dermatitis include soaps and detergents.
Potential allergens that can cause contact dermatitis include:
Contact dermatitis presents with blistered or scaly, erythematous plaques, which are often irregular in shape and sharply demarcated. Patients may give a history of exposure to a relevant irritant or allergen. Systemic symptoms and signs are absent.

Contact dermatitis

Contact dermatitis

Contact dermatitis
Panniculitis refers to a group of conditions in which there is subcutaneous inflammation of fat. Panniculitis is characterised by red, firm, tender plaques or nodules that have a predilection for the lower legs.
The most common form of panniculitis is erythema nodosum, which can be distinguished from cellulitis by its bilateral and multifocal distribution, recurrent nature, and absence of oedema. Patients may have systemic symptoms, either from an underlying cause, or from the panniculitis itself, which can cause fever, malaise, and arthralgia.



Lupus panniculitis
Lymphoedema is a common mimic of cellulitis. The underlying pathogenesis of lymphoedema is similar to venous disease, in which there is decreased tissue oxygenation as a result of extravasated lymph.
Clinical features of lymphoedema include:
The inguinal lymphatics may have been damaged or occluded by filariasis, lymph node dissection, radiation therapy, or obesity. Infectious signs and symptoms are absent.
Lymphoedema is associated with a risk of cutaneous infection, including cellulitis, due to impaired lymphatic drainage.



Eosinophilic cellulitis, or Wells syndrome, is characterised by recurrent itchy or painful plaques of unknown cause in which prominent eosinophils are found on skin biopsy. A minority of patients with eosinophilic cellulitis may experience malaise and fevers but multiple lesions and the recurring history should distinguish it from cellulitis. Plaques are usually bright red at first, then fade over 4–8 weeks, leaving green, grey, or brown patches.

Wells syndrome

Wells syndrome

Wells syndrome
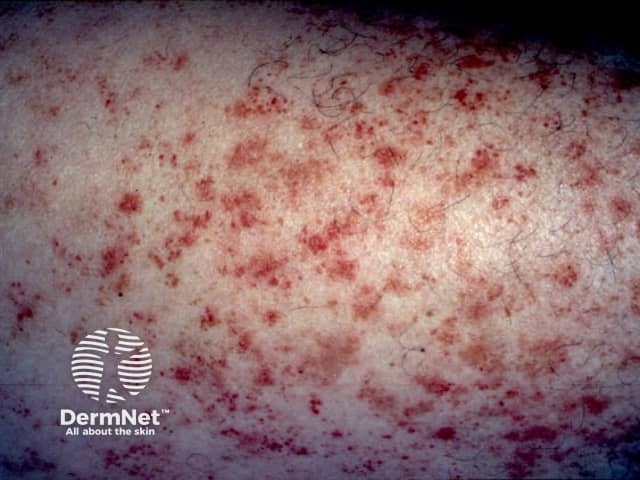
Small vessel vasculitis is characterised by painful erythematous plaques and palpable purpura. It most often affects both lower legs. There are various causes.
Vasculitis can be accompanied by ulceration, blistering and mild systemic symptoms such as fever and malaise. Multiple and non-blanching lesions distinguish it from cellulitis. Biopsy will usually show leukocytoclastic vasculitis.

Small vessel vasculitis

Small vessel vasculitis

Small vessel vasculitis
Capillaritis may be unilateral or bilateral, acute, chronic or recurrent. It favours the lower legs. It is characterised by 'cayenne-pepper' petechiae, but these may resemble cellulitis when confluent and accompanied by erythematous patches and oedema. The leg is cool and there are no systemic symptoms.


Rare mimics of cellulitis include:

Carcinoma erysipeloides

Erythromelalgia

Periodic fever