Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
First created in 1997. Updated by Dr Gayle Ross, Dermatologist, Melbourne Hospital, Melbourne, VIC, Australia. DermNet Editor in Chief Adjunct A/Prof. Amanda Oakley, Dermatologist, Hamilton, New Zealand. March 2019.
Introduction - porphyrias Introduction Demographics Clinical features Diagnosis Treatment Outlook
The porphyrias are a group of metabolic conditions which can be either genetic or acquired. The porphyrin pathway is involved in haem synthesis. Haem is the red pigment in haemoglobin in blood cells and carries oxygen in the blood. A deficiency or block of one of the enzymes in the porphyrin pathway results in a build-up of the corresponding precursor protein or intermediate molecule.
The porphyrias can be broadly classified as acute or cutaneous.
Porphyria cutanea tarda (PCT) is the most common type of porphyria.
The symptoms of PCT are limited to the skin. It does not cause people to become acutely unwell, as in the acute types of porphyria.
PCT is caused by a defect in a liver enzyme uroporphyrinogen decarboxylase (UROD).
It is hereditary in one-third of patients when there is usually a family history of the condition and symptoms begin in early adult life.
In other patients, PCT is due to underlying liver disease and patients present with symptoms in their 40s and 50s. The liver diseases associated with PCT include:
Hormones such as oral contraceptive or hormone replacement therapy may also trigger PCT.
Renal dialysis patients can also develop PCT as they cannot excrete the porphyrins.
Rarely, other conditions such as systemic lupus erythematosus (SLE) and human immunodeficiency virus (HIV) infection can cause PCT.
Many patients have more than one risk factor.
Excess porphyrin in the skin results in photosensitivity. Individuals with PCT present with increasingly fragile skin on the back of the hands and the forearms. Other sun-exposed sites such as the face, scalp, neck, and arms may also be affected.
Features include:
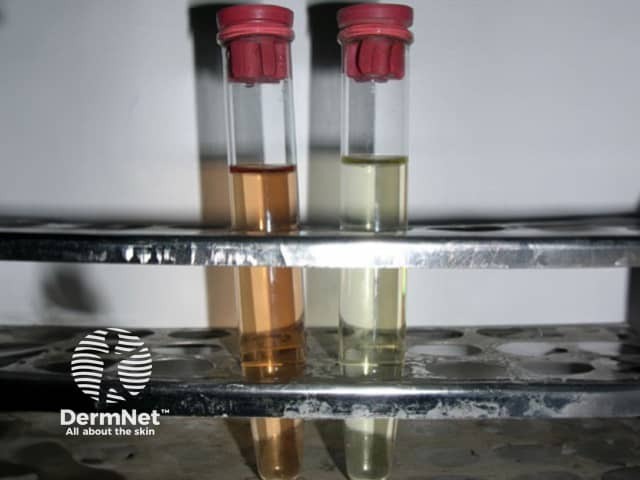
Characteristically, the urine is darker than usual, with a reddish or tea-coloured hue.

Porphyria cutanea tarda

Porphyria cutanea tarda

Porphyria cutanea tarda

Porphyria cutanea tarda

Porphyria cutanea tarda
Porphyria cutanea tarda
PCT may be clinically suspected but should always be confirmed by laboratory tests.
Tests to determine the cause of the porphyria may include:
Treatment of an underlying liver problem may result in the resolution of PCT and may include reducing alcohol consumption, stopping oestrogen or hormone treatment, avoiding excessive iron intake, or antiviral treatment for underlying hepatitis C.
Once clear, PCT is unlikely to recur unless the underlying risk factors have not been addressed. If PCT is ongoing, there can be an increased risk of liver cancer.