Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1998. Updated by Dr Ebtisam Elghblawi, Dermatologist, Tripoli, Libya. DermNet Editor in Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. August 2019.
Introduction
Introduction - diabetes mellitus
Diabetic dermopathy
Diabetic bullae
Diabetic stiff skin
Other dermatological conditions associated with diabetes
It is estimated that 30% of patients with diabetes mellitus will experience a skin problem at some stage throughout the course of their disease. Several skin disorders are more common in diabetic patients, particularly those due to infection such as candida and impetigo. Patients with type 2 diabetes also have twice the risk of developing the common scaly disease, psoriasis, as non-diabetics.

Impetigo

Candida intertrigo

Psoriasis
Specific skin conditions associated with diabetes mellitus are described below.
Diabetes mellitus constitutes a collection of diverse disorders associated with an increase in blood glucose concentration.
Diabetes is associated with impaired carbohydrate, protein, and fat metabolism due to insufficient secretion of insulin or target-tissue insulin resistance. Complications of diabetes mellitus comprise both macrovascular (cardiovascular) and microvascular (retinopathy, nephropathy, or neuropathy) sequelae.
Type 1 diabetes mellitus is characterised by absolute insulin absence and is due to autoimmune beta-cell destruction. It typically presents with acute symptoms or ketoacidosis in childhood or adolescence, and lifelong insulin therapy is mandatory.
Type 2 diabetes mellitus is a common disorder categorised by insulin resistance and relative insulin deficiency. Patients are often asymptomatic and are diagnosed through screening. Strong risk factors include older age, obesity, physical inactivity, prior gestational diabetes, pre-diabetes, non-white ancestry, family history of diabetes, and polycystic ovary syndrome. Modification of cardiovascular risk factors (eg, hypertension and dyslipidaemia) are an important part of treatment, along with glycaemic control to prevent microvascular complications.
Type 2 diabetes is the main cause of type 2 diabetes in children, who are usually over 10 years of age. Acanthosis nigricans accompanies childhood diabetes in 90–95%.
Gestational diabetes is diagnosed if glucose intolerance is first recognised during pregnancy at 24–28 weeks of gestation. Strong risk factors include advanced maternal age (more than 40 years), obesity, personal history of gestational diabetes or macrosomia affecting a previous child, polycystic ovary syndrome, non-white ancestry, and a family history of diabetes mellitus.
Other presentations of diabetes mellitus include diabetic ketoacidosis, hyperosmolar hyperglycaemic state, diabetic cardiovascular disease, diabetic kidney disease, diabetic neuropathy, diabetic foot, diabetic retinopathy, and metabolic syndrome.
The increasing prevalence of diabetes requires targeted screening for detecting diabetes and prediabetes in risk groups to prevent and mitigate the progression of the disease.
Diabetic dermopathy is a skin condition characterised by light brown or reddish, oval or round, slightly indented scaly patches most often appearing on the shins. Although these lesions may appear in anyone, particularly after an injury or trauma to the area, they are one of the most common skin problems found in patients with diabetes mellitus. Diabetic dermopathy has been found to occur in up to 30% of patients with diabetes.
Diabetic dermopathy is sometimes also referred to as shin spots and pigmented pretibial patches. They resemble solar lentigines.

Diabetic dermopathy

Diabetic dermopathy

Diabetic dermopathy
The exact cause of diabetic dermopathy is unknown but may be associated with diabetic neuropathic and vascular complications, as studies have shown the condition to occur more frequently in diabetic patients with retinopathy, neuropathy and nephropathy.
Diabetic dermopathy tends to occur in older patients or those who have had diabetes for at least 10–20 years. It also appears to be closely linked to increased glycosylated haemoglobin, an indicator of poor control of blood glucose levels.
Because lesions often occur over bony parts of the body such as the shins, it is thought that diabetic dermopathy may also be a magnified response to injury or trauma to these areas. Studies have shown that shin spots have appeared in response to trauma with heat, cold or blunt objects in patients with diabetes.
Diabetic dermopathy lesions appear most frequently on the shins. Less commonly lesions can be found on the front of the thighs, forearm, side of the foot, scalp and trunk. Features of lesions are:
The presence of four or more lesions is almost always limited to patients with diabetes. People presenting with shin spots not already diagnosed with diabetes should undergo a further investigation to rule out the possibility of early diabetes.
Diabetic dermopathy lesions or shin spots are harmless. They usually do not require any treatment and tend to go away after a few years, particularly following improved blood glucose control.
Diabetic bullae, also known as bullosis diabeticorum, are blister-like lesions that occur spontaneously on the feet and hands of diabetic patients. Although rare, diabetic bullae are a distinct marker for diabetes.
The blisters are painless and can be from 0.5–17 centimetres in size. They often have an irregular shape. Two types of diabetic bullae have been defined.
In most cases, diabetic bullae heal spontaneously without treatment. Patients should make sure the blister remains unbroken to avoid secondary infection.

Diabetic bullae

Diabetic bullae

Diabetic bullae
Many patients with longstanding type 1 diabetes develop diabetic cheiroarthropathy or diabetic stiff skin (digital sclerosis). This results in restricted mobility of the joints of their hands and stiff, waxy, thickened and yellowed skin. This is thought to be due to the reaction of glucose with proteins in the skin and increased glycation end products. These patients may also suffer from Dupuytren contracture (tendon tightening, which bends the fingers).

Diabetic stiff skin

Diabetic stiff skin
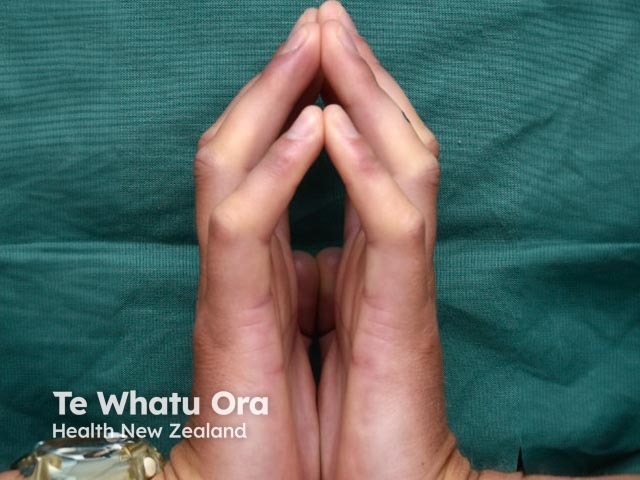
Diabetic stiff skin
Other common conditions in diabetics are foot ulcers and necrobiosis lipoidica.
Diabetics with renal failure are also prone to reactive perforating collagenosis and Kyrle disease.

Scleredema

Generalised granuloma annulare

Eruptive xanthoma

Xanthelasma

Skin tag

Vitiligo

Acanthosis nigricans

Necrobiosis lipoidica

Excoriations due to pruritus

Boil

Cellulitis

Candida intertrigo