Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Last Reviewed: August, 2024
Author(s): Dr Tristen Ng, Dermatology Resident, Royal Perth Hospital, Australia (2024)
Peer reviewed by: Dr Emily Wales, UK; Dr Libby Whittaker, Medical Writer, NZ (2024)
Previous contributors: Hon A/Prof Amanda Oakley, Dermatologist, New Zealand (2014)
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outcome
Folliculitis keloidalis, also called folliculitis keloidalis nuchae (FKN), is a chronic scarring folliculitis of the occipital scalp. It mostly affects men of African-Caribbean descent with black curly hair.
Folliculitis keloidalis is commonly called acne keloidalis nuchae (AKN), although the condition is not related to acne vulgaris, and the scars formed are not true keloid scars. Dermatitis papillaris capillitii is another synonym.

Small papules and nodules with overlying alopecia due to FKN

A pustule evident within an area of FKN

Papules and alopecia on the nape of the neck in FKN
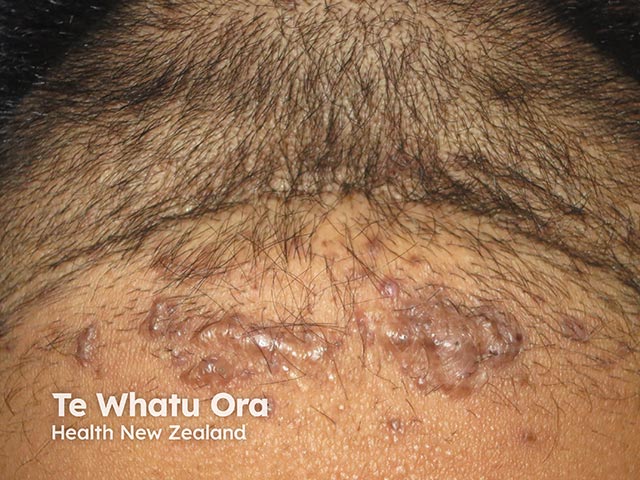
Papules, nodules and keloid like scars on the nape

Dense scarring alopecia and tufting over the nape in advanced FKN
View more images of folliculitis keloidalis
Folliculitis keloidalis mostly affects men of African-Caribbean descent with afro-textured hair, and may also affect men of Hispanic, Middle Eastern, Mediterranean, Asian, and Pacific descent. It is 20 times more common in men than women.
Onset occurs after adolescence and is rare after the age of 55 years.
Folliculitis keloidalis may occur in combination with other inflammatory conditions such as acne inversa (hidradenitis suppurativa), dissecting scalp cellulitis, pilonidal disease, and acne conglobata.
The exact pathophysiology of folliculitis keloidalis is poorly understood but is thought to be exacerbated by mechanical injury and an aberrant immune response. Potential contributing factors include:
Other disorders reported to be associated with folliculitis keloidalis include metabolic syndrome, gout, hidradenitis suppurativa, and keratosis follicularis spinulosa decalvans.
View images of folliculitis keloidalis
The keloid-like scars may range from dark pink to dark brown or black in colour. Postinflammatory hyperpigmentation from papules and pustules is common in darker Fitzpatrick skin types (eg, III to VI).
Folliculitis keloidalis is a clinical diagnosis based on the findings of papules, pustules, and keloid-like plaques on the occipital scalp and nape of the neck.
Biopsy is rarely necessary unless the diagnosis is equivocal. If there is uncertainty, consider a punch biopsy, ideally including a suspected keloidal papule and the base of the hair follicle. The histology of folliculitis keloidalis nuchae is characteristic, should a biopsy be performed.
Other investigations may be indicated depending on the differential diagnoses and/or suspected complications eg, fungal or bacterial culture.
Folliculitis keloidalis can be challenging to treat, and there are no consensus guidelines regarding management. Early diagnosis and intervention can help to prevent progression and reduce scarring and hair loss. The following measures may be helpful.
Mild to moderate cases:
Moderate to severe cases:
If limited response to treatment (or extensive disease), consider:
Secondary infection can complicate folliculitis keloidalis and may require additional antimicrobial therapy (guided by swab results). Intralesional corticosteroid administration is usually delayed until active bacterial infection is resolved.
While it isn’t known how to completely prevent folliculitis keloidalis in the first place, one of the key aims of management is to prevent disease progression by:
Folliculitis keloidalis should be treated early to ensure the best cosmetic outcome. If left untreated, the acneiform lesions may eventually converge and form large keloid-like scars, making treatment more challenging.