Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Latest update by Dr Alexis Daniel Lara Rivero, Dermatologist, Hospital Universitario de Caracas, Venezuela. Reviewed by Dr Margot Whitfeld, Dermatologist, Sydney, Australia. DermNet Editor in Chief: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. December 2017.
Introduction
Demographics
Causes
Clinical features
Complications
Differential diagnoses
Outcome
Mycetoma is a chronic infection of the skin and the subcutaneous tissue. It can sometimes also affect muscles, bones, tendons and joints.
Mycetoma is characterised by nodules and sinus tracts that discharge watery fluid or pus containing grains [1].
Mycetoma is classified as:

Mycetoma foot

Courtesy Dr. Sriyani Samaraweera

Actinomycetoma due to nocardia
The bacteria and fungi causing mycetoma have a worldwide distribution in the soil and plant material, but mycetoma is mostly found in tropical areas in south and south-east Asia, Latin America and Africa. Most cases are reported in the ‘Trans-African mycetoma belt” from western Africa, including Senegal and Sierra Leone, to eastern Africa, including Somalia and Sudan [2,3].
Infection usually occurs after local trauma.
Mycetoma has no known vector or animal reservoir, and there are no reports of infections transmitted from person to person [1,3].
The causative agent can be suspected from the colour of the grains.
Dark or black grains
White, pail or unstained grains
White to yellow grains
Brown grains
Red to pink grains
The incubation time after inoculation of the microorganism until mycetoma is diagnosed ranges from months to years [2].
Actinomycetoma and eumycetoma have similar clinical features. However, actinomycetomas tend to be more aggressive and destructive, invading bones earlier.
Mycetoma has little effect on the general condition of the affected patient and fever is rare [2].

Actinomycetoma foot and legs
Complications of mycetoma include:
These can be prevented by early diagnosis and proper treatment [4].
Mycetoma is suspected when there is a typical triad of symptoms and signs:
Dermoscopy may be useful for early stages of the disease detecting grains within skin lesions [5]. Grains are conglomerates of fungi or bacteria disposed radially (like sun rays).
Tissue for microscopy and culture is collected by:
The colour of the grains can narrow the options of the causative bacterium or fungus. The grains are treated with potassium hydroxide (KOH) and then stained with Gram and PAS stains. On microscopy:
As some are slow-growing organisms, cultures at 25–30°C and 37°C are set for up to 6 weeks for both bacteria and fungi [1,6]. When it is difficult to identify the responsible organism, molecular techniques such as PCR (polymerase chain reaction) can be used [2].
Skin biopsy may show typical histopathological features of mycetoma.
Imaging can be used to assess the depth of infection [6].
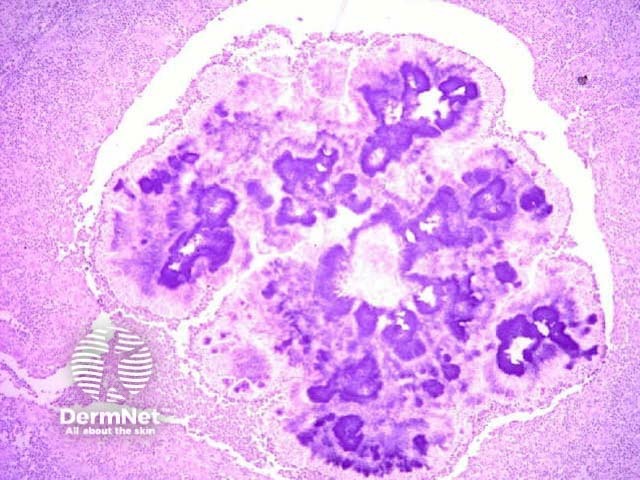
H&E stain of actinomycosis grains
Infectious diseases
Non-infectious diseases
Mycetoma cannot be cured without active treatment. It requires antibiotics (for actinomycetomas) or oral antifungals (for eumycetomas) for weeks, months or years. Damage to subcutaneous tissues (muscle, bones, joints or tendons) often persists, so local surgery (including amputation) and physiotherapy may be required [1,2].
Actinomycetoma (single or in combination)
Eumycetoma (only one usually used)
Despite the need for prolonged treatment, prognosis is usually good with proper therapy. The longer the infection has been present prior to treatment, the more likely complications and disability will occur [4].