Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Dr Ebtisam Elghblawi, Specialist Dermatologist, Tripoli, Libya (2022); Dr Amy Stanway, Dermatologist, New Zealand (2004).
Reviewing dermatologist: Dr Ian Coulson
Edited by the DermNet content department
Introduction
Demographics
Causes
Clinical features
Variation in skin types
Complications
Diagnosis
Differential diagnoses
Treatment
Prevention
Outcome
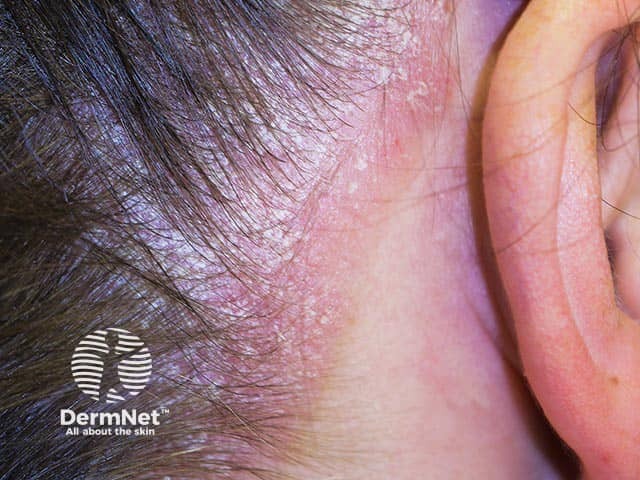
Scalp psoriasis is a skin condition characterised by red, thickened, well-demarcated patches or plaques with overlying silvery-white scales, affecting part or all of the scalp.
It can be contained within the hairline, though frequently affects the back of the head, or extends onto the forehead (facial psoriasis), ears, or neck. While often camouflaged by the hair, scalp psoriasis can be a source of embarrassment and distress due to itching and dandruff-like flaking. It may occur in isolation, or with any other form of psoriasis, and is typically a chronic, relapsing-remitting condition.

Scalp psoriasis extending beyond the anterior hairline
Confluent psoriasis in the scalp extending anteriorly from the hairline

Marked thick scaling in psoriasis of the scalp

Extensive scaling over the parietal scalp due to psoriasis. There is psoriasis also in the ears and around the hair line

Marked scaling in psoriasis of the scalp

Severe scalp psoriasis with areas of pityriasis amianticea
Psoriasis is estimated to affect 2% of the population worldwide and can occur at any age. Among those affected by psoriasis, approximately 80% experience scalp involvement.
In psoriasis, skin cells tend to form quickly (hyperproliferation), within days rather than weeks, due to faulty immune system signals. As a result, excess cells pile up on the skin surface, causing patches and plaques.
Psoriasis, including scalp psoriasis, is thought to be caused and affected by a combination of genetic, immune, hormonal, and environmental factors, such as:
According to Gelfand et al (2005), the prevalence of all psoriasis was 1.3% in black patients compared to 2.5% in white patients, which is probably linked to genetics.
However, the diagnosis of psoriasis may also be delayed or missed in darker skin phototypes where the presentation of psoriasis may vary from purple to dark brown patches with grey or silver scales.
When managing scalp psoriasis in patients with different skin and hair types, it is important to formulate a topical treatment regimen that is compatible with each patient’s hair care practices and cultural preferences. For example, hair texture that requires a reduced frequency of hair washing thereby renders daily medicated shampoos unsuitable. Once weekly washing in conjunction with daily application of a topical corticosteroid in a vehicle compatible with preferred hair styling practices may be more acceptable.
Scalp psoriasis is generally diagnosed clinically. Key trichoscopic findings include red dots, hairpin vessels, and red globular rings (for more information, see trichoscopy of inflammatory conditions). A skin biopsy may be performed in some cases to confirm the diagnosis.
Additionally, assessing psoriasis severity — for example, using the Psoriasis Scalp Severity Index (PSSI) — and its impact on quality-of-life is important.
Scalp psoriasis can be difficult to treat due to the delivery of therapy in and around the hair, which complicates the application of many topical products. Cosmetic considerations also affect treatment adherence.
Usually, lotions, solutions, or gels are more suitable for the scalp than heavier products such as ointments. In recent years, a number of new formulations have been developed (eg, foams, shampoos, and sprays) that enhance cosmetic acceptability and adherence. Most treatments will need to be used regularly for several weeks before a benefit is seen, and may have to be applied regularly to keep the scalp clear.
See Treatment of psoriasis for more information.
Topical medications are recommended as first-line treatment of mild-to-moderate scalp psoriasis, and can also be used concomitantly with phototherapy and/or systemic therapies in moderate-to-severe cases.
Consider first-line for patients with scalp psoriasis and accompanying moderate-to-severe whole-body psoriasis; and second-line in other cases where there has been an inadequate response to topical therapy.
Support groups can also be helpful for those living with psoriasis.
Scalp psoriasis tends to be a chronic problem. However, regular scalp care, maintenance treatment, lifestyle factors, and avoiding triggers or exacerbating factors can help prevent or reduce the severity of flares.
While scalp psoriasis is generally a chronic, relapsing-remitting condition, there are many available treatment options. The mainstay of treatment is topical therapy, although this can be challenging for scalp conditions given their location and the presence of hair.
Newer topical formulations, such as foams and sprays, can help to improve treatment tolerability and outcomes. In patients with moderate-to-severe disease who do not respond to topical treatments, there are a number of systemic therapies including immunomodulatory agents and biological treatments.