Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Authors: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1998. Updated September 2015. Further updated: Dr Gaurav Dhawan, Dermatology Specialty Trainee, Salford Royal Hospital United Kingdom. Copy edited by Gus Mitchell. March 2022
Introduction
Demographics
Causes
Clinical features
Diagnosis
Differential diagnoses
Treatment
Outlook
Pyoderma gangrenosum (PG) presents as a rapidly enlarging, very painful ulcer. It is one of a group of autoinflammatory disorders known as neutrophilic dermatoses.
The name pyoderma gangrenosum is historical. The condition is not an infection (pyoderma), nor does it cause gangrene.
It is characterised by a full-thickness ulcer with blue/purple undermined borders and by pathergy.
Pyoderma gangrenosum is a rare disease that affects males and females of any age but is more common in those aged over 50 years. It frequently is associated with an internal disease or condition. Its known associations include:
About half of those affected by pyoderma gangrenosum have none of the associated risk factors.
IBD-associated pyoderma gangrenosum has the following characteristics:
Pyoderma gangrenosum is an autoinflammatory disease (excessive response to an internal antigen) due to some form of neutrophil dysfunction. T lymphocytes and cytokines are involved. There may be a genetic predisposition.
Drugs are occasionally implicated as triggers of pyoderma gangrenosum, especially cocaine, isotretinoin, propylthiouracil, and sunitinib (a protein kinase inhibitor).
Injury to the skin is a common trigger (the pathergic response), and a surgical trigger is well known, and often misinterpreted as a wound infection.
Untreated, the ulcers may continue to enlarge, persist unchanged, or may slowly heal. Treatment is usually successful in arresting the process, but complete healing may take months. This is particularly true if there is an underlying venous disease, another reason for leg ulcers.
Deep ulcers heal with scarring, and this is sometimes with a characteristic cribriform (criss-cross pattern) or atrophic appearance. There are several rarer subtypes of pyoderma gangrenosum:

Early haemorrhagic pyoderma gangrenosum

Ulceration, pustulation and the violaceos edge of pyoderma gangrenosum on the shin associated with ulcerative colitis

Bullous pyoderma gangrenosum with underlying ulcerative colitis

The erythematous and violaceous border typical of pyoderma gangrenosum above the knee

Multiple ulcers on the shin - the superior edge of the proximal ulcer showing the characterisitc purple edge
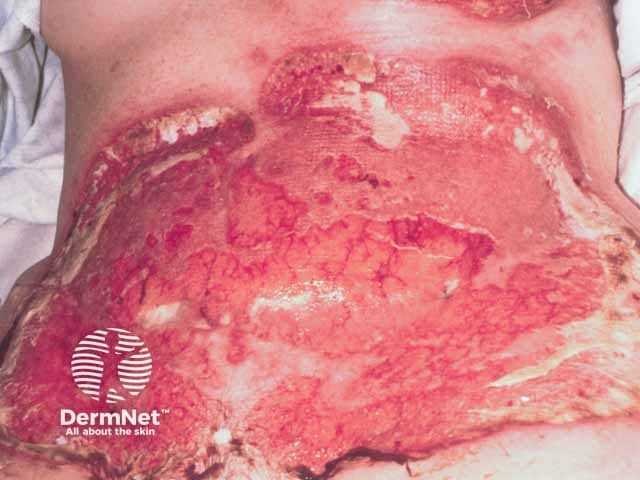
Severe pathergic pyoderma gangrenosum after breast cancer reconstructive surgery (TRAM procedure) (PG-patient1)

Healed post operative pyoderma gangrenosum after pulse intravenous methylprednisolone and ciclosporin (PG-patient1)

Multiple ulcers on the buttocks - note the violaceous oedematous ulcer edges
Pyoderma gangrenosum is diagnosed by its characteristic appearance and severe pain. The pathergy test is usually positive (a skin prick test causing a papule, pustule, or ulcer).
Criteria published after a Delphi consensus exercise in 2018 supersede the Su criteria with a single major criterion required to diagnose pyoderma gangrenosum (a neutrophilic infiltrate). The addition of four or more of the eight minor criteria yields a sensitivity of 86% and a specificity of 90% for pyoderma gangrenosum.
Several other ulcerating conditions can mimic pyoderma gangrenosum such as:
Treatment of pyoderma gangrenosum is mainly non-surgical. The necrotic tissue should be gently removed. Wide surgical debridement should be avoided during the active stage of pyoderma gangrenosum because it may result in enlargement of the ulcer. Skin grafting and other surgical procedures may be performed when the active disease phase has settled, with care to minimise trauma.
Often conventional antibiotics such as flucloxacillin are prescribed before making the correct diagnosis. These may be continued if bacteria are cultured in the wound (secondary wound infection) or there is surrounding cellulitis (red hot, painful skin), but they are not helpful for uncomplicated pyoderma gangrenosum.
Small ulcers are often treated with:
Systemic treatment for larger ulcers due to pyoderma gangrenosum may include:
Other therapies may include:
Expert wound care and pain management are essential. Once the disease is stable and inactive, surgical repair may be considered using a skin flap, skin graft, negative pressure wound therapy, and cultured skin.
Systemic therapy should be tapered slowly over several months.
The prognosis for pyoderma gangrenosum is unpredictable. About half of treated patients achieve wound healing on treatment with prednisone or ciclosporin within a year.
Patients with pyoderma gangrenosum should be very careful to avoid trauma, which can set off a new ulcer.