Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Reactions Treatments Lesions (cancerous)
Authors: Sarah Friske and Dr Riyad N.H. Seervai, Baylor College of Medicine, United States of America. Copy edited by Gus Mitchell. July 2022.
Introduction
Introduction - targeted anticancer therapies
Targets
Cutaneous adverse effects
The advent of targeted cancer therapies, including monoclonal antibodies and small-molecule inhibitors, has initiated an era of precision medical oncology focused on targeting vulnerabilities specific to cancer cells.
All modalities of anticancer therapy have the risk of causing substantial cutaneous toxicities that can seriously affect a patient’s quality of life.
Traditional chemotherapy utilises nonspecific properties of cytotoxic agents to impede cell division. Alternatively, the discovery of cancer-associated gene mutations and hallmark-related signal transduction pathways has allowed physicians to treat cancer in a more precise manner.
Monoclonal antibodies (Mabs) target factors related to the induction of apoptosis and cell death, and prevention of angiogenesis and growth factor signalling. Recently, Mabs have been effective at leveraging the immune system to avert cancer through immune checkpoint inhibition.
An assortment of small-molecule inhibitors (Nibs) have been approved to target pathways associated with the most distinctive features of cancer leading to superior overall/progression-free survival outcomes and a reduced adverse-effect profile compared with that of chemotherapy.
The mitogen-activated protein (MAP) kinase pathway promotes cancer survival, proliferation, angiogenesis, migration, and invasion. Frequent anticancer targets of this pathway include the protein kinases BRAF and MEK.
BRAF mutations are found in ~50% of melanomas. The first two BRAF inhibitors, vemurafenib and dabrafenib, are associated with significant improvement in progression-free and overall survival in patients with metastatic melanoma.
Adverse cutaneous reactions include:

Keratoacanthoma
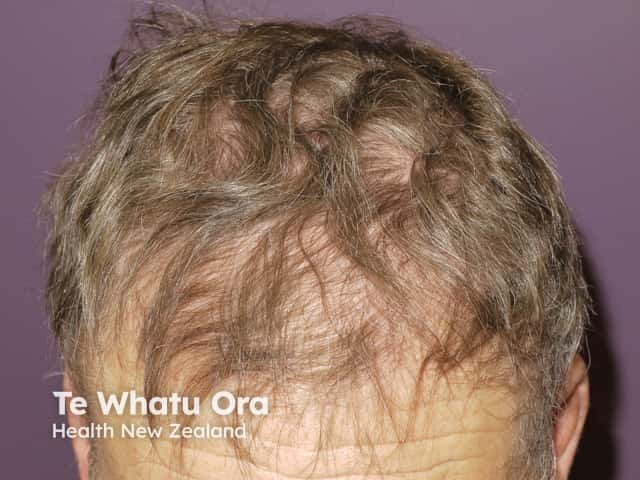
Alopecia due to vemurafenib

Folliculitis due to vemurafenib
Trametinib, selumetinib, cobimetinib, and binimetinib are MEK inhibitors currently in use.
Adverse cutaneous reactions include:
Anticancer therapies target receptor tyrosine kinase signalling pathways via inhibition of multikinases VEGF, EGFR, and FGFR.
Multikinase inhibitors currently include sorafenib, sunitinib, axitinib, regorafenib, lenvatinib, and vandetanib.
Adverse cutaneous reactions include:
VEGF is key in moderating tumorigenesis by promoting the development of abnormal vasculature around the tumour. Current therapies targeting VEGF include bevacizumab, regorafenib, and lenvatinib.
The most common dermatologic toxicities are:

Hand-foot reaction

Photosensitivity
Epidermal growth factor receptor (EGFR) signalling causes downstream activation of the heterodimeric lipid kinase phosphatidylinositol-3-kinase (PI3K) and AKT. Current therapies inhibiting the resulting cell proliferation include gefitinib, erlotinib, icotinib, dacomitinib, afatinib, osimertinib, poziotinib, mobocertinib, alpelisib, ipatasertib, capivasertib, and uprosertib.
The most common dermatologic toxicities are:
For more information, see cutaneous side effects of EGFR and protein kinase inhibitors.
Alterations in the fibroblast growth factor receptor (FGFR) family of tyrosine kinases have been linked to ~7% of all human cancers. Therapies targeting FGFR include erdafitinib, rogaratinib, futibatinib, infigratinib, pemigatinib, derazantinib, Debio 1347, and isogatinib.
Adverse cutaneous reactions include:
Hallmarks of cancer associated with cell division include genomic instability, evading growth suppression, and replicative immortality. Common anticancer therapeutic targets associated with cell division and DNA repair include PARP and CDK4/6.
The poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP) enzyme is involved in DNA repair via nucleotide and base excision repair. Therapies targeting PARP include olaparib, rucaparib, talazoparib, niraparib, and veliparib.
Adverse cutaneous reactions include:
The G1 to S phase transition of the cell cycle is driven by cyclin-dependent kinases 4 and 6 (CDK4/6). Current anticancer therapies include abemaciclib, ribociclib, and palbociclib.
Dermatologic toxicities associated with CDK4/6 inhibitors are rare. A combination trial with aromatase inhibitor therapy reported a higher rate of rash, alopecia, pruritus, and stomatitis in the CDK4/6 and aromatase inhibitor group compared to placebo.
Targeted cancer therapy for myeloproliferative disorders utilize BCR-ABL inhibitors and Janus kinase inhibitors.
Chronic myeloid leukaemia (CML) is a myeloproliferative neoplasm, resulting from the Philadelphia (Ph) chromosome balanced translocation, associated with the BCR-ABL fusion oncoprotein. Imatinib is a current therapy that targets BCR-ABL.
Cutaneous adverse reactions include:
Primary myelofibrosis and polycythemia vera are frequently associated with mutation of the Janus kinase 2 (JAK2) non-receptor tyrosine kinase (V617F). Ruxolitinib is a current anticancer Janus kinase inhibitor.
Adverse cutaneous reactions include: